What Is Abruptio Placentae
PLACENTA ABRUPTION
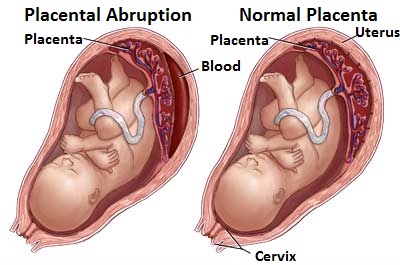
Placenta abruption is also known as abruptio placentae or premature separation of the placenta.
Risk factors of placenta abruption are hypertension (greatest association),trauma, polyhydramnios, multifetal gestation,
smoking, use of crack cocaine, chorioamnionitis,preterm premature rupture of membranes and Rapid decompression of uterine cavity, as can occur in polyhydramnios or multifetal gestation.
The etiology of placenta abruption are hypertension: found in 40% to 50% of grade III abruptions, Blunt external trauma (motor vehicle accident, spousal abuse) and
Abruptio placentae is the separation of placenta from the uterine wall before delivery of the fetus. There are three classes of abruption based on maternal and fetal status, including an assessment of uterine contractions, quantity of
bleeding, fetal heart rate monitoring, and abnormal coagulation studies (fibrinogen, prothrombin time, partial thromboplastin time).
Grade I: mild vaginal bleeding, uterine irritability, stable vital signs, reassuring fetal heartrate, normal coagulation profile(fibrinogen 450 mg%) , Grade II: moderate vaginal bleeding, hypertonic uterine contractions, orthostatic blood
pressure measurements, unfavorable fetal status, fibrinogen 150 to 250 mg% and Grade III: severe bleeding (may be concealed),hypertonic uterine contractions, overt signs of hypovolemic shock, fetal death, thrombocytopenia,
fibrinogen < 150 mg%
The symptoms and signs of placenta abruption are Triad of uterine bleeding (concealed or per vagina), hypertonic uterine contractions or signs of preterm labor, and evidence of fetal compromise exists. More than 80% of cases have external bleeding , 20% of cases have no bleeding but have indirect evidence of abruption, such as failed tocolysis for preterm labor. Tetanic uterine contractions are found in only 17% of cases unless grade II or III abruption.
The differential diagnosis of placenta abruption are placenta previa, rupture of membranes cervical or vaginal trauma, labor,cervical cancer and membranes rupture.
Investigation required are Baseline hemoglobin and hematocrit help to quantify blood loss and establish baseline
values for serial comparisons during expectant management, coagulation profile: platelets, fibrinogen, prothrombin,
and partial thromboplastin time,Diffuse intravascular coagulation can develop with severe abruption. If fibrinogen is ,150
mg%, estimated blood loss is approximately 2000 ml; if fibrinogen is ,100 mg%, consider fresh frozen plasma to prevent further bleeding and type and antibody screen is important to identify Rh-negative patients who may need Rh immune globulin. Ultrasound should include fetal presentation and status, amniotic fluid volume, placental location,as well as any evidence of hematoma (retroplacental, subchorionic, or preplacental).
The treatment may include initial assessment should evaluate for the source of bleeding, ruling out placenta previa that may contraindicate any type of vaginal examination (e.g., pelvic speculum examination), continuous fetal heart monitoring is indicated for all viable gestations (60% incidence offetal distress in labor); may show early signs of maternal hypovolemia (late decelerations or fetal tachycardia) before overt maternal vital sign changes. Actual amount of blood loss is often greater than initially perceived because of the possibility of concealed retroplacental bleedinand apparent “normal” vital signs. The relative hypervolemia of pregnancy initially protects the patient until late in the course of
bleeding, when abrupt and sudden cardiovascular collapse can occur
Stabilization of the mother is the first priority. Treatment depends on gestational age of the fetus, severity of the abruption, and maternal status. Initial assessment for signs of maternal hemodynamic compromise or hemorrhagic
shock; large-bore intravenous access, with crystalloid fluid resuscitation using a replacement of 3 ml lactated Ringer’s solution for every 1 ml estimated blood loss. ndwelling Foley catheter to monitor urine output and maternal volume status, with a goal of 30 ml/hr urine output. Assess fetal status and gestational age by
sonogram and continuous fetal heart rate monitoring. Because of the unpredictable nature of abruptions,
cross-matched blood should be made available during the initial resuscitation period.
In the term fetus or when lung maturity has been documented, delivery is indicated. In the preterm fetus or a fetus with an immature lung profile, consider betamethasone 12.5 mg IM q24h for two doses and then delivery, depending on the severity of the abruption and the likelihood of fetal complication from preterm birth. Cesarean section should be reserved for cases of fetal distress or for standard obstetric indications. While Cesarean delivery may be needed to stabilize the fetal and/or maternal status, the mother’s coagulation status may complicate the procedure and availability of blood products may be critical. In select cases, such as severe prematurity with a stable mother and mild contractions,magnesium sulfate can be used for tocolysis, 6 g IV loading dose then 3 g/hr maintenance,
to allow for course of steroids.
Placenta abruption is also known as abruptio placentae or premature separation of the placenta.
Risk factors of placenta abruption are hypertension (greatest association),trauma, polyhydramnios, multifetal gestation,
smoking, use of crack cocaine, chorioamnionitis,preterm premature rupture of membranes and Rapid decompression of uterine cavity, as can occur in polyhydramnios or multifetal gestation.
The etiology of placenta abruption are hypertension: found in 40% to 50% of grade III abruptions, Blunt external trauma (motor vehicle accident, spousal abuse) and
Abruptio placentae is the separation of placenta from the uterine wall before delivery of the fetus. There are three classes of abruption based on maternal and fetal status, including an assessment of uterine contractions, quantity of
bleeding, fetal heart rate monitoring, and abnormal coagulation studies (fibrinogen, prothrombin time, partial thromboplastin time).
Grade I: mild vaginal bleeding, uterine irritability, stable vital signs, reassuring fetal heartrate, normal coagulation profile(fibrinogen 450 mg%) , Grade II: moderate vaginal bleeding, hypertonic uterine contractions, orthostatic blood
pressure measurements, unfavorable fetal status, fibrinogen 150 to 250 mg% and Grade III: severe bleeding (may be concealed),hypertonic uterine contractions, overt signs of hypovolemic shock, fetal death, thrombocytopenia,
fibrinogen < 150 mg%
The symptoms and signs of placenta abruption are Triad of uterine bleeding (concealed or per vagina), hypertonic uterine contractions or signs of preterm labor, and evidence of fetal compromise exists. More than 80% of cases have external bleeding , 20% of cases have no bleeding but have indirect evidence of abruption, such as failed tocolysis for preterm labor. Tetanic uterine contractions are found in only 17% of cases unless grade II or III abruption.
The differential diagnosis of placenta abruption are placenta previa, rupture of membranes cervical or vaginal trauma, labor,cervical cancer and membranes rupture.
Investigation required are Baseline hemoglobin and hematocrit help to quantify blood loss and establish baseline
values for serial comparisons during expectant management, coagulation profile: platelets, fibrinogen, prothrombin,
and partial thromboplastin time,Diffuse intravascular coagulation can develop with severe abruption. If fibrinogen is ,150
mg%, estimated blood loss is approximately 2000 ml; if fibrinogen is ,100 mg%, consider fresh frozen plasma to prevent further bleeding and type and antibody screen is important to identify Rh-negative patients who may need Rh immune globulin. Ultrasound should include fetal presentation and status, amniotic fluid volume, placental location,as well as any evidence of hematoma (retroplacental, subchorionic, or preplacental).
The treatment may include initial assessment should evaluate for the source of bleeding, ruling out placenta previa that may contraindicate any type of vaginal examination (e.g., pelvic speculum examination), continuous fetal heart monitoring is indicated for all viable gestations (60% incidence offetal distress in labor); may show early signs of maternal hypovolemia (late decelerations or fetal tachycardia) before overt maternal vital sign changes. Actual amount of blood loss is often greater than initially perceived because of the possibility of concealed retroplacental bleedinand apparent “normal” vital signs. The relative hypervolemia of pregnancy initially protects the patient until late in the course of
bleeding, when abrupt and sudden cardiovascular collapse can occur
Stabilization of the mother is the first priority. Treatment depends on gestational age of the fetus, severity of the abruption, and maternal status. Initial assessment for signs of maternal hemodynamic compromise or hemorrhagic
shock; large-bore intravenous access, with crystalloid fluid resuscitation using a replacement of 3 ml lactated Ringer’s solution for every 1 ml estimated blood loss. ndwelling Foley catheter to monitor urine output and maternal volume status, with a goal of 30 ml/hr urine output. Assess fetal status and gestational age by
sonogram and continuous fetal heart rate monitoring. Because of the unpredictable nature of abruptions,
cross-matched blood should be made available during the initial resuscitation period.
In the term fetus or when lung maturity has been documented, delivery is indicated. In the preterm fetus or a fetus with an immature lung profile, consider betamethasone 12.5 mg IM q24h for two doses and then delivery, depending on the severity of the abruption and the likelihood of fetal complication from preterm birth. Cesarean section should be reserved for cases of fetal distress or for standard obstetric indications. While Cesarean delivery may be needed to stabilize the fetal and/or maternal status, the mother’s coagulation status may complicate the procedure and availability of blood products may be critical. In select cases, such as severe prematurity with a stable mother and mild contractions,magnesium sulfate can be used for tocolysis, 6 g IV loading dose then 3 g/hr maintenance,
to allow for course of steroids.