|
|
Pathology definition - Autoimmune Hemolytic Anemia
Autoimmune hemolytic anemia
There are two forms of autoimmune hemolytic anemia. These include cold agglutinin disease and warm antibody autoimmune hemolytic anemia.
Cold agglutinin disease may present with hemolytic anemia. In later stage, it may progress into jaundice. On exposure to cold weather the patient may develop mild hemolytic anemia. Patient is advised to avoid any cold exposure. Cold agglutinin disease is caused by the reaction of the IgM antibodies against the I antigen on the red blood cells. This will finally lead to phagocytosis of the red blood cell. IgM antibodies are triggered by infection such as mycoplasma pneumonia, infectious mononucleosis or by Waldenstrom macroglobulinemia.
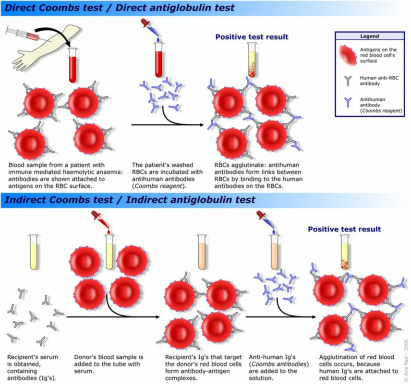
The investigation required include Coomb test to detect the present of antibodies on the the surface of the patient’s red blood cell. The peripheral blood film/peripheral blood smear may reveal reticulocytosis or spherocytes. Patient may present with positive cold agglutinin test.
Warm antibody autoimmune hemolytic anemia may present with splenomegaly and hemolytic anemia and jaundice ( severe in nature). Warm antibody autoimmune hemolytic anemia may occur due to reaction of the IgG antibodies on the membrane of the red blood cell. IgG antibodies are associated with lymphoma, chronic lymphocytic leukemia and systemic lupus erythematosus.
The investigation may include Coomb test to detect the present of antibodies on the surface of the patient’s red blood cell. The peripheral blood film/peripheral blood smear may reveal reticulocytosis and spherocytes. Patient may also present with positive direct Coomb test with a decreased in the level of the hematocrit. The treatments required for warm antibody autoimmune hemolytic anemia are splenectomy and prednisolone.
Other causes of autoimmune hemolytic anemia may include drugs intake such as methyldopa or penicillin.
References
1. Gehrs, Bradley C., and Richard C. Friedberg. “Autoimmune Hemolytic Anemia.” American Journal of Hematology 69, no. 4 (2002): 258–271. doi:10.1002/ajh.10062.
2.Dacie JV. “AUtoimmune Hemolytic Anemia.” Archives of Internal Medicine 135, no. 10 (October 1, 1975): 1293–1300. doi:10.1001/archinte.1975.00330100019004.
There are two forms of autoimmune hemolytic anemia. These include cold agglutinin disease and warm antibody autoimmune hemolytic anemia.
Cold agglutinin disease may present with hemolytic anemia. In later stage, it may progress into jaundice. On exposure to cold weather the patient may develop mild hemolytic anemia. Patient is advised to avoid any cold exposure. Cold agglutinin disease is caused by the reaction of the IgM antibodies against the I antigen on the red blood cells. This will finally lead to phagocytosis of the red blood cell. IgM antibodies are triggered by infection such as mycoplasma pneumonia, infectious mononucleosis or by Waldenstrom macroglobulinemia.
The investigation required include Coomb test to detect the present of antibodies on the the surface of the patient’s red blood cell. The peripheral blood film/peripheral blood smear may reveal reticulocytosis or spherocytes. Patient may present with positive cold agglutinin test.
Warm antibody autoimmune hemolytic anemia may present with splenomegaly and hemolytic anemia and jaundice ( severe in nature). Warm antibody autoimmune hemolytic anemia may occur due to reaction of the IgG antibodies on the membrane of the red blood cell. IgG antibodies are associated with lymphoma, chronic lymphocytic leukemia and systemic lupus erythematosus.
The investigation may include Coomb test to detect the present of antibodies on the surface of the patient’s red blood cell. The peripheral blood film/peripheral blood smear may reveal reticulocytosis and spherocytes. Patient may also present with positive direct Coomb test with a decreased in the level of the hematocrit. The treatments required for warm antibody autoimmune hemolytic anemia are splenectomy and prednisolone.
Other causes of autoimmune hemolytic anemia may include drugs intake such as methyldopa or penicillin.
References
1. Gehrs, Bradley C., and Richard C. Friedberg. “Autoimmune Hemolytic Anemia.” American Journal of Hematology 69, no. 4 (2002): 258–271. doi:10.1002/ajh.10062.
2.Dacie JV. “AUtoimmune Hemolytic Anemia.” Archives of Internal Medicine 135, no. 10 (October 1, 1975): 1293–1300. doi:10.1001/archinte.1975.00330100019004.
