Chest pain causes

chest pain causes
The aim of this article to:
Chest pain is one of the most common presenting symptoms or complaints that has to seen by physician. There are a lot of causes of chest pain and because of this a thorough history should be taken from the patient. Some of the causes of pain in the chest will lead to fatality and require quick management and diagnosis while others are considered benign. It is important as the first step to divide the causes of chest pain into cardiac causes and non cardiac causes.
When the patient present with chest pain a few points need to address while asking the patient which may include :
-the site of the pain ( lateral, central or posterior )
-onset of the pain ( continuous or intermittent)
-the duration of the pain
-burning, crushing or stabbing in characteristic
-exaggerating factors such as posture, eating, breathing, movement, emotion, exertion or
food intake.
-radiation of the pain ( arm , neck , jaw)
-severity of the pain ( effort tolerance). How far can the patient walk on the flat line or
the number of stairs the patient manage to climb before suffering chest pain
Past medical history is an important question to ask. Pay particular attention on the following questions.
-Any history of hypertension ( high risk factor for dissection of thoracic aorta and pericarditis)
-Any history of recent surgery that may be complicated by other disorders such as mediastinitis, pulmonary embolism, ischemic heart disease and viral pericarditis.
-Any history of long period of immobility ( malignancy, surgery, long flight ) which is a risk factors for developing pulmonary embolism.
-Any history of recent viral infection ( pericarditis )
-Any history of ingestion of non steroids anti inflammatory drugs or peptic ulcer disease
-Any history of ischemic heart disease.
Other important factors that need to be focus including identifying the patient smoking status and any positive family history of ischemic heart disease. History of alcohol intake provides an information regarding the risk factors of peptic ulcer disease and gastritis. Thrombolysis is one of the treatment in cardiac cause of chest pain such as in acute coronary syndrome, however thormbolysis is contraindicated in the treatment of dissection of the thoracic aorta and pericarditis. Carful history is required to identify the present of pericarditis and dissection of the thoracic aorta.
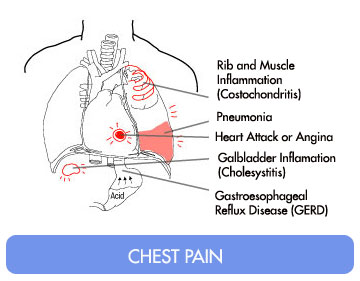
DIfferential diagnosis of chest pain may include:
Cardiac causes of chest pain
Angina pectoris, myocardial infarction, pericarditis, myocarditis and mitral valve prolapsed.
Vascular causes of chest pain
Dissection of the thoracic aorta
Respiratory causes of chest pain
Pulmonary neoplasm, pulmonary embolism, pneumonia and pneumothorax.
Neurological causes of chest pain
Herpes zoster
Musculoskeletal causes of chest pain
Tiezte syndrome, costochondritis, muscular spasm, fractured rib and compression of cervical nerve root by cervical disc.
Gastrointestinal causes of chest pain
Biliary disease, esophagitis, gastroesophageal reflux, esophageal spasm esophageal tear, and peptic ulcer disease.
The most common cause of chest pan may include myocardial ischemia, pericarditis, aortic dissection, gastrointestinal causes and musculoskeletal pain.
Myocardial ischemia is presented with crushing,band or tight like pain which is present on the anterior part of the chest and radiated to the arm, neck, jaw, teeth and back. It is exacerbated with exertion, emotion, anxious, food, cold air, and movement and relieves with glyceryl trinitrate and resting The associated features may include breathlessness, shock, sweaty and nausea.
Pericarditis is presented with sharp pain which in selected cases may be crushing in character. Pericarditis is presented on the anterior sides of the heart and no radiation is present. It is worse on lying flat but better while leaning forward. It is presented arthralgia ( joint pain), recent viral illness and fever.
Aortic dissection is presented with sharp, tearing, and stabbing pain which present on the retrosternal at the interscapular region and no radiation of the pain. It is present continuously with no evidence of exacerbating or relieving factors. It is associated with radio femoral delay in pulses, unequal blood pressure or pulses on both arm. on auscultation aortic regurgitant murmur may be heard.
Musculoskeletal pain can present everywhere in the chest region. It is radiated to both of the arm , to the front or back. It is sharp and dull ache in characteristic. It will get worst with movement of the neck or pressing of the chest wall. It is associated in selected cases with pain in the joint ( arthralgia).
Gastrointestinal causes of chest pain present on the center of the chest and it is radiated to the throat in selected cases. It is burning in characteristic and make worst with food in case of esophageal pain and relived with food or antacid in case of peptic ulcer disease or cholecystitis.
Pleuritic pain is also associated with chest pain. It is presented as a sharp/crushing pain that occur everywhere on the chest region and appear to be more localized than other causes of chest pain. It has not radiated to other part of the body. The exacerbating factors may include breathing, movement, coughing and posture but relieved with resting. The associated features may include cough, hemoptysis, breathlessness and shock in case the patient suffer from pulmonary embolism.
General examination of the patient with chest pain may include cardiovascular, respiratory and gastrointestinal systems.
Initial examination may include inspection of the patient. Look for any signs of shock such as sweating or pallor which suggest dissection of the aorta, myocardial infarction and pulmonary embolism. The present of labour breathing is suggestive of pneumonia and left ventricular infarction. Look also for any evidence of coughing which suggest pneumonia and left ventricular failure as well as any obvious history of vomiting.
Cardiovascular examination may include feeling the pulse and blood pressure. Feel for any evidence of regularity of the rhythm and rates of the pulses either it is tachycardia and bradycardia. The blood pressure is measured and any evidence of hypertension or hypotension is recorded. The blood pressure and pulses are also measured on both hand to look for any evidence of inequality that suggest dissection of the aorta. The waveform of the carotid pulses is feel, slow rising pulse is associated with aortic stenosis due to angina and collapsing pulses due to aortic regurgitation associated with dissection of the aorta. Raised jugular venous pressure is suggestive of pulmonary embolism or right ventricular failure. The pale mucous membrane suggestive of anemia due to angina or cyanosis that suggestive of hypoxia. The anterior part of the chest is palpate and feel for any abnormal impulses on the chest that suggest a paradoxical movement that present on the anterior myocardial infarction. Auscultate the heart and listen for the first, second, third heart sound, pericardial rub, mitral and aortic regurgitation ( indication of dissection of the aorta and myocardial infarction) as well as aortic stenosis ( angina ).
The respiratory examination may include observation for any signs of breathlessness and cyanosis. On palpation , there is an unequal expansion of the thorax and on percussion there is a dullness on the lung region. On auscultation, pleural rub and bronchial breathing may be detected ( pneumonia).
On gastrointestinal examination, the patient typically complain of generalized abdominal guarding and tenderness. The absent of bowel sound suggest peptic ulcer disease and peritonitis.
Investigation may include blood test, ECG, chest radiography, echocardiography, CT scan , MRI scan and ventilation perfusion scan as well as exercise tolerance test and myocardial perfusion scan.
The blood test may include full blood count. The present of anemia in full blood count may exacerbate angina. Urea and electrolytes and renal function test are useful to inspect for any evidence of dehydration or hypokalemia due to diuretic therapy and vomiting. Cardiac biomarker such as creatine kinase or cardiac troponin I or troponin T that is used to risk stratify patient with cardiac causes of chest pain. ( Acute coronary syndrome).Amylase and liver function test may be useful to detect cholecystitis or peptic ulcer disease. Hypocapnoea in arterial blood gases reading may suggest hyperventilation while hypoxia suggest left ventricular function and pulmonary embolism.
The electrocardiography test or ECG is used to define the heart rates and rhythm. Any abnormalities detected is associated with cardiac causes of chest pain. The elevation of the ST interval without any evidence of bundle branch block is indicated of acute cases of myocardial infarction which is exacerbated from the Prinzmental angina. Any cases of ST depression without bundle branch block is associated with myocardial ischemia. If the ST depression is detected while the patient was exercising that it is associated with tachyarrhythmias as well as exertion induced angina. ST depression that occur while resting is associated with non Q wave myocardial infarction and unstable angina. The present of Q wave indicates the present of old myocardial infarction which occur more than 24 hours. The pattern of atrial fibrillation indicates the present of pulmonary disease and myocardial ischemia. The new onset of bundle branch block indicates the new onset of myocardial infarction.
Any cases of large pulmonary embolism is presented with sinus tachycardia/atrial fibrillation,tall P wave on lead II ,( right atrium dilation), right axis deviation, right bundle branch block , present of S waves on lead I , Q waves on lead III and inverted T wave on lead III.
In patient suffers from chest pain, chest x ray investigation may reveals widening of the mediastinum ( aortic dissection), cardiomegaly, lung lesion, oligaemic lung field ( pulmonary embolism), pleural or pericardial effusion.
Echocardiography may reveal abnormalities of the mitral and aortic valve ( aortic dissection or myocardial infarction) , abnormalities/ dissection of the aorta with the present of the false lumen, pericardial effusion which suggest dissection and pericarditis and any regional abnormalities of the myocardial function which is significant with myocardial infarction and myocardial ischemia.
Computed tomography or magnetic resonance imaging is useful in urgent case where aortic dissection is suspected (high sensitivity). It is also useful to detect any case of large pulmonary embolism by using large spiral computed tomography.
Ventilation perfusion scan is useful to exclude any present of pulmonary embolism. However if pulmonary embolism is still highly suspected then CT pulmonary angiogram is perform.
If angina is suspected in later stage is advisable for the patient to undergoes the myocardial perfusion scan and exercise tolerance test.
In emergency setting for the patient who present with chest pain, the series of investigation that are required may include:
ECG-any abnormalities will require further attention. If the ECG is normal then myocardial infarction is excluded.
Chest X ray - any abnormalities such as widening of the mediastinum is indicated of aortic dissection. Any consolidation or effusion is highly suggestive of pulmonary causes of chest pain such as pneumonia or pneumothorax.
Cardiac biomarker such as troponin I or troponin T or creatine kinase is also useful. The result may be normal for the first 4 hour before it start to rise. If the level of cardiac troponin is less than 0.06 microgram/l then the 5 month risk of mortality is around 4. 3% l(low risk). If the level of troponin is around 0.06 -0.18 microgram /l then the 5 year risk is 10.5% (medium risk) and 16.1% if the level of troponin is more than 0.18 microgram/l ( high risk).
As a summary if the patient complain of chest pain while resting ,the next step is to perform and ECG test and look at the reading. If there is an ST elevation myocardial infarction is considered. If there is a concave ST elevation, pericarditis is highly suggestive and if there is ST depression with T wave inversion and flattening further test is require which include exercise ECG, coronary angiogram, serial ECG or chemical biomarker test).
If the chest pain occur on exertion then angina is suspected. Further test such as exercise ECG or coronary angiogram is performed.
Chest pain which is sharp in characteristic and occur on inspiration is highly suspected of pulmonary causes of chest pain such as Dressler syndrome, pulmonary embolism, pulmonary neoplasm , pneumonia and pneumothorax.
Chest pain that may also be associated with musculoskeletal causes such as central chest pain that is associated with esophagitis or lateral chest pain which is associated with shingles or herpes zoster.
An ST elevation on the ECG indicates that there is an obstruction of the proximal coronary epicardial artery. If remain untreated, myocardial necrosis will develop and finally leads to left ventricular damage (without restoration of coronary blood flow).The treatment may include angioplasty and thrombolysis.
Thrombolysis or fibrinolytic therapy is a form of treatment for ischemic heart disease. However a few safety precaution should be noted before this form of treatment is commenced. There are a few absolute contraindication that should be remember such as any history of stroke of unknown origin or hemorrhagic stroke, ischemic storke for the past 6 months, gastrointestinal bleeding within a months, trauma, head injury and bleeding for the last 3 weeks, bleeding disorder, aortic dissection and any central nervous system neoplasm or damage. The relative contraindication may includes, 1 week postpartum, pregnancy, prolonged traumatic resuscitation, non compressive punctures, systolic blood pressure more than 180mmHg /refractory hypertension, active peptic ulcer disease, advanced liver disease and infective endocarditis, transient ischemic attack for the last 6 months and patient on oral anticoagulant therapy.
There are also a certain condition where thrombolysis is contraindicated such as pulmonary embolism, mediastinitis, pericarditis, dissection of the thoracic aorta. Pulmonary embolism may present as an acute chest pain in an ill patient and intermittent chest pain in a healthy individual. There are a lot of causes of chest pain that may include immobility due to prolonged bed rest or long journey, postoperative which may include leg, hip, pelvic and abdominal surgery, hypercoagulable state which include oral contraceptive pill, malignancy and protein C as well as protein S deficiency and hemoconcentration may include polycythemia and diuretic therapy. Venous stasis due to poor flow of venous blood is associated with atrial fibrillation due to the formation of thrombus in the right ventricular and atrial fibrillation.
The patient who suffer from pulmonary embolism may present with dyspnea, localized chest pain, coughing, hemoptysis , sweating, hypotensive , sudden collapse, syncope which follow with cardiac arrest. The ECG may reveals a sinus rhythm with electromechanical dissociation or tachyarrhythmias. Pulmonary embolism caries the risk of 10 percent mortality. The treatment may include, infusion of intravenous heparin or subcutaneous low molecular weight heparin. Warfarin is useful for pulmonary embolism that is confirmed.
Mediastinitis
It is an unusual disorder which is only suspected when there is an esophageal tear which is detected on during esophageal surgery and endoscopy.
Pericarditis
Patient present with sharp or crushing chest pain that is located on the central anterior of the chest. There is no radiation of the pain and the pain is aggravating by lying forward or breathing movement. There is an evidence of prodromal illness such as fever or arthralgia.
On auscultation, pericarditis is presented with pericardial rub which is scratchy in quality which can be heard in the ear. The complication of pericarditis may include the formation of the pleural effusion. This is presented with impalpable cardiac impulse. The patient may also present with globular heart shadow in the chest X ray. The ECG may reveal an ST elevation which is concave is shaped in all leads except lead AVR. It is contraindicated for thrombolysis as it may leads to hemipericardium.
Dissection of the thoracic aorta
The predisposing factors for developing dissection of the thoracic aorta may include pregnancy, hypertension, bicuspid aortic valve, middle age men, connective tissue disorder SLE , Ehlers- Danlos syndrome as well as Marfan syndrome, Noonan syndrome and Turner syndrome.
The pathophysiology of dissection of the aorta may include an increase in the intraluminal pressure which leads to a damage to the tunica media and causing an intimal tear.The luminal plane of the tunica media is entered and dissect which later lead to a creation of false lumen. Aortic dissection is classified according to the Stanford Classification. Stanford classification type A involved ascending aorta while Stanford classification type B involved other part than ascending aorta.
Patient presented with central stabbing, sharp , tearing pain which later radiates to the back /interscapular retrosternum. The pain is continuous and constant. If the disscetion involve the coronary ostia then myocardial infarction may occur. Hemiplegia, dysphasia and paraplegia are associated with dissection that involved the spinal arteries. Mesenteric arteries are associated with abdominal pain.
Patient may also presented with breathlessness, shock , cyanosed and sweating. There will be an unequal pulse and blood pressure on both arms and legs with radio - radial delay or radio- femoral delay. Other complication may include cardiac failure, cardiac tamponade and aortic regurgitation.
The investigation requires may include ECG that reveal ST elevation , Chest X ray that reveals widening of the mediastinum with fluid in the costophrenic angle, MRI, CT scan that may reveal false lumen and echocardiography which is the best investigation method which may shows pericardial effusion.
The treatment of dissection of the thoracic aorta may include the administration of the pain reliever such as diamorphine. This is follow by establishing an intravenous access through the central and arterial line. Fluid replacement therapy is followed by the administration of colloid solution and blood. Cross match 10 unit of blood is required. The next step involved to control the blood pressure which involved the infusion of the sodium nitroprusside or labetalol infusion if no evidence of cardiac failure to maintain the blood pressure 120/80mmHg. Surgical approach is only require in cases where the dissection is type A and medical management, percutaneous treatment or surgical approach is suitable for type B aortic dissection based on the Stanford classification.
The aim of this article to:
- help us in getting the history from the patient who complain of chest pain.
- guide us in formulating the complete differential diagnosis of chest pain.
- perform a complete physical examination on the patient presenting with chest pain.
- order specific test / investigation to rule out the underlying cause of chest pain.
Chest pain is one of the most common presenting symptoms or complaints that has to seen by physician. There are a lot of causes of chest pain and because of this a thorough history should be taken from the patient. Some of the causes of pain in the chest will lead to fatality and require quick management and diagnosis while others are considered benign. It is important as the first step to divide the causes of chest pain into cardiac causes and non cardiac causes.
When the patient present with chest pain a few points need to address while asking the patient which may include :
-the site of the pain ( lateral, central or posterior )
-onset of the pain ( continuous or intermittent)
-the duration of the pain
-burning, crushing or stabbing in characteristic
-exaggerating factors such as posture, eating, breathing, movement, emotion, exertion or
food intake.
-radiation of the pain ( arm , neck , jaw)
-severity of the pain ( effort tolerance). How far can the patient walk on the flat line or
the number of stairs the patient manage to climb before suffering chest pain
Past medical history is an important question to ask. Pay particular attention on the following questions.
-Any history of hypertension ( high risk factor for dissection of thoracic aorta and pericarditis)
-Any history of recent surgery that may be complicated by other disorders such as mediastinitis, pulmonary embolism, ischemic heart disease and viral pericarditis.
-Any history of long period of immobility ( malignancy, surgery, long flight ) which is a risk factors for developing pulmonary embolism.
-Any history of recent viral infection ( pericarditis )
-Any history of ingestion of non steroids anti inflammatory drugs or peptic ulcer disease
-Any history of ischemic heart disease.
Other important factors that need to be focus including identifying the patient smoking status and any positive family history of ischemic heart disease. History of alcohol intake provides an information regarding the risk factors of peptic ulcer disease and gastritis. Thrombolysis is one of the treatment in cardiac cause of chest pain such as in acute coronary syndrome, however thormbolysis is contraindicated in the treatment of dissection of the thoracic aorta and pericarditis. Carful history is required to identify the present of pericarditis and dissection of the thoracic aorta.
DIfferential diagnosis of chest pain may include:
Cardiac causes of chest pain
Angina pectoris, myocardial infarction, pericarditis, myocarditis and mitral valve prolapsed.
Vascular causes of chest pain
Dissection of the thoracic aorta
Respiratory causes of chest pain
Pulmonary neoplasm, pulmonary embolism, pneumonia and pneumothorax.
Neurological causes of chest pain
Herpes zoster
Musculoskeletal causes of chest pain
Tiezte syndrome, costochondritis, muscular spasm, fractured rib and compression of cervical nerve root by cervical disc.
Gastrointestinal causes of chest pain
Biliary disease, esophagitis, gastroesophageal reflux, esophageal spasm esophageal tear, and peptic ulcer disease.
The most common cause of chest pan may include myocardial ischemia, pericarditis, aortic dissection, gastrointestinal causes and musculoskeletal pain.
Myocardial ischemia is presented with crushing,band or tight like pain which is present on the anterior part of the chest and radiated to the arm, neck, jaw, teeth and back. It is exacerbated with exertion, emotion, anxious, food, cold air, and movement and relieves with glyceryl trinitrate and resting The associated features may include breathlessness, shock, sweaty and nausea.
Pericarditis is presented with sharp pain which in selected cases may be crushing in character. Pericarditis is presented on the anterior sides of the heart and no radiation is present. It is worse on lying flat but better while leaning forward. It is presented arthralgia ( joint pain), recent viral illness and fever.
Aortic dissection is presented with sharp, tearing, and stabbing pain which present on the retrosternal at the interscapular region and no radiation of the pain. It is present continuously with no evidence of exacerbating or relieving factors. It is associated with radio femoral delay in pulses, unequal blood pressure or pulses on both arm. on auscultation aortic regurgitant murmur may be heard.
Musculoskeletal pain can present everywhere in the chest region. It is radiated to both of the arm , to the front or back. It is sharp and dull ache in characteristic. It will get worst with movement of the neck or pressing of the chest wall. It is associated in selected cases with pain in the joint ( arthralgia).
Gastrointestinal causes of chest pain present on the center of the chest and it is radiated to the throat in selected cases. It is burning in characteristic and make worst with food in case of esophageal pain and relived with food or antacid in case of peptic ulcer disease or cholecystitis.
Pleuritic pain is also associated with chest pain. It is presented as a sharp/crushing pain that occur everywhere on the chest region and appear to be more localized than other causes of chest pain. It has not radiated to other part of the body. The exacerbating factors may include breathing, movement, coughing and posture but relieved with resting. The associated features may include cough, hemoptysis, breathlessness and shock in case the patient suffer from pulmonary embolism.
General examination of the patient with chest pain may include cardiovascular, respiratory and gastrointestinal systems.
Initial examination may include inspection of the patient. Look for any signs of shock such as sweating or pallor which suggest dissection of the aorta, myocardial infarction and pulmonary embolism. The present of labour breathing is suggestive of pneumonia and left ventricular infarction. Look also for any evidence of coughing which suggest pneumonia and left ventricular failure as well as any obvious history of vomiting.
Cardiovascular examination may include feeling the pulse and blood pressure. Feel for any evidence of regularity of the rhythm and rates of the pulses either it is tachycardia and bradycardia. The blood pressure is measured and any evidence of hypertension or hypotension is recorded. The blood pressure and pulses are also measured on both hand to look for any evidence of inequality that suggest dissection of the aorta. The waveform of the carotid pulses is feel, slow rising pulse is associated with aortic stenosis due to angina and collapsing pulses due to aortic regurgitation associated with dissection of the aorta. Raised jugular venous pressure is suggestive of pulmonary embolism or right ventricular failure. The pale mucous membrane suggestive of anemia due to angina or cyanosis that suggestive of hypoxia. The anterior part of the chest is palpate and feel for any abnormal impulses on the chest that suggest a paradoxical movement that present on the anterior myocardial infarction. Auscultate the heart and listen for the first, second, third heart sound, pericardial rub, mitral and aortic regurgitation ( indication of dissection of the aorta and myocardial infarction) as well as aortic stenosis ( angina ).
The respiratory examination may include observation for any signs of breathlessness and cyanosis. On palpation , there is an unequal expansion of the thorax and on percussion there is a dullness on the lung region. On auscultation, pleural rub and bronchial breathing may be detected ( pneumonia).
On gastrointestinal examination, the patient typically complain of generalized abdominal guarding and tenderness. The absent of bowel sound suggest peptic ulcer disease and peritonitis.
Investigation may include blood test, ECG, chest radiography, echocardiography, CT scan , MRI scan and ventilation perfusion scan as well as exercise tolerance test and myocardial perfusion scan.
The blood test may include full blood count. The present of anemia in full blood count may exacerbate angina. Urea and electrolytes and renal function test are useful to inspect for any evidence of dehydration or hypokalemia due to diuretic therapy and vomiting. Cardiac biomarker such as creatine kinase or cardiac troponin I or troponin T that is used to risk stratify patient with cardiac causes of chest pain. ( Acute coronary syndrome).Amylase and liver function test may be useful to detect cholecystitis or peptic ulcer disease. Hypocapnoea in arterial blood gases reading may suggest hyperventilation while hypoxia suggest left ventricular function and pulmonary embolism.
The electrocardiography test or ECG is used to define the heart rates and rhythm. Any abnormalities detected is associated with cardiac causes of chest pain. The elevation of the ST interval without any evidence of bundle branch block is indicated of acute cases of myocardial infarction which is exacerbated from the Prinzmental angina. Any cases of ST depression without bundle branch block is associated with myocardial ischemia. If the ST depression is detected while the patient was exercising that it is associated with tachyarrhythmias as well as exertion induced angina. ST depression that occur while resting is associated with non Q wave myocardial infarction and unstable angina. The present of Q wave indicates the present of old myocardial infarction which occur more than 24 hours. The pattern of atrial fibrillation indicates the present of pulmonary disease and myocardial ischemia. The new onset of bundle branch block indicates the new onset of myocardial infarction.
Any cases of large pulmonary embolism is presented with sinus tachycardia/atrial fibrillation,tall P wave on lead II ,( right atrium dilation), right axis deviation, right bundle branch block , present of S waves on lead I , Q waves on lead III and inverted T wave on lead III.
In patient suffers from chest pain, chest x ray investigation may reveals widening of the mediastinum ( aortic dissection), cardiomegaly, lung lesion, oligaemic lung field ( pulmonary embolism), pleural or pericardial effusion.
Echocardiography may reveal abnormalities of the mitral and aortic valve ( aortic dissection or myocardial infarction) , abnormalities/ dissection of the aorta with the present of the false lumen, pericardial effusion which suggest dissection and pericarditis and any regional abnormalities of the myocardial function which is significant with myocardial infarction and myocardial ischemia.
Computed tomography or magnetic resonance imaging is useful in urgent case where aortic dissection is suspected (high sensitivity). It is also useful to detect any case of large pulmonary embolism by using large spiral computed tomography.
Ventilation perfusion scan is useful to exclude any present of pulmonary embolism. However if pulmonary embolism is still highly suspected then CT pulmonary angiogram is perform.
If angina is suspected in later stage is advisable for the patient to undergoes the myocardial perfusion scan and exercise tolerance test.
In emergency setting for the patient who present with chest pain, the series of investigation that are required may include:
ECG-any abnormalities will require further attention. If the ECG is normal then myocardial infarction is excluded.
Chest X ray - any abnormalities such as widening of the mediastinum is indicated of aortic dissection. Any consolidation or effusion is highly suggestive of pulmonary causes of chest pain such as pneumonia or pneumothorax.
Cardiac biomarker such as troponin I or troponin T or creatine kinase is also useful. The result may be normal for the first 4 hour before it start to rise. If the level of cardiac troponin is less than 0.06 microgram/l then the 5 month risk of mortality is around 4. 3% l(low risk). If the level of troponin is around 0.06 -0.18 microgram /l then the 5 year risk is 10.5% (medium risk) and 16.1% if the level of troponin is more than 0.18 microgram/l ( high risk).
As a summary if the patient complain of chest pain while resting ,the next step is to perform and ECG test and look at the reading. If there is an ST elevation myocardial infarction is considered. If there is a concave ST elevation, pericarditis is highly suggestive and if there is ST depression with T wave inversion and flattening further test is require which include exercise ECG, coronary angiogram, serial ECG or chemical biomarker test).
If the chest pain occur on exertion then angina is suspected. Further test such as exercise ECG or coronary angiogram is performed.
Chest pain which is sharp in characteristic and occur on inspiration is highly suspected of pulmonary causes of chest pain such as Dressler syndrome, pulmonary embolism, pulmonary neoplasm , pneumonia and pneumothorax.
Chest pain that may also be associated with musculoskeletal causes such as central chest pain that is associated with esophagitis or lateral chest pain which is associated with shingles or herpes zoster.
An ST elevation on the ECG indicates that there is an obstruction of the proximal coronary epicardial artery. If remain untreated, myocardial necrosis will develop and finally leads to left ventricular damage (without restoration of coronary blood flow).The treatment may include angioplasty and thrombolysis.
Thrombolysis or fibrinolytic therapy is a form of treatment for ischemic heart disease. However a few safety precaution should be noted before this form of treatment is commenced. There are a few absolute contraindication that should be remember such as any history of stroke of unknown origin or hemorrhagic stroke, ischemic storke for the past 6 months, gastrointestinal bleeding within a months, trauma, head injury and bleeding for the last 3 weeks, bleeding disorder, aortic dissection and any central nervous system neoplasm or damage. The relative contraindication may includes, 1 week postpartum, pregnancy, prolonged traumatic resuscitation, non compressive punctures, systolic blood pressure more than 180mmHg /refractory hypertension, active peptic ulcer disease, advanced liver disease and infective endocarditis, transient ischemic attack for the last 6 months and patient on oral anticoagulant therapy.
There are also a certain condition where thrombolysis is contraindicated such as pulmonary embolism, mediastinitis, pericarditis, dissection of the thoracic aorta. Pulmonary embolism may present as an acute chest pain in an ill patient and intermittent chest pain in a healthy individual. There are a lot of causes of chest pain that may include immobility due to prolonged bed rest or long journey, postoperative which may include leg, hip, pelvic and abdominal surgery, hypercoagulable state which include oral contraceptive pill, malignancy and protein C as well as protein S deficiency and hemoconcentration may include polycythemia and diuretic therapy. Venous stasis due to poor flow of venous blood is associated with atrial fibrillation due to the formation of thrombus in the right ventricular and atrial fibrillation.
The patient who suffer from pulmonary embolism may present with dyspnea, localized chest pain, coughing, hemoptysis , sweating, hypotensive , sudden collapse, syncope which follow with cardiac arrest. The ECG may reveals a sinus rhythm with electromechanical dissociation or tachyarrhythmias. Pulmonary embolism caries the risk of 10 percent mortality. The treatment may include, infusion of intravenous heparin or subcutaneous low molecular weight heparin. Warfarin is useful for pulmonary embolism that is confirmed.
Mediastinitis
It is an unusual disorder which is only suspected when there is an esophageal tear which is detected on during esophageal surgery and endoscopy.
Pericarditis
Patient present with sharp or crushing chest pain that is located on the central anterior of the chest. There is no radiation of the pain and the pain is aggravating by lying forward or breathing movement. There is an evidence of prodromal illness such as fever or arthralgia.
On auscultation, pericarditis is presented with pericardial rub which is scratchy in quality which can be heard in the ear. The complication of pericarditis may include the formation of the pleural effusion. This is presented with impalpable cardiac impulse. The patient may also present with globular heart shadow in the chest X ray. The ECG may reveal an ST elevation which is concave is shaped in all leads except lead AVR. It is contraindicated for thrombolysis as it may leads to hemipericardium.
Dissection of the thoracic aorta
The predisposing factors for developing dissection of the thoracic aorta may include pregnancy, hypertension, bicuspid aortic valve, middle age men, connective tissue disorder SLE , Ehlers- Danlos syndrome as well as Marfan syndrome, Noonan syndrome and Turner syndrome.
The pathophysiology of dissection of the aorta may include an increase in the intraluminal pressure which leads to a damage to the tunica media and causing an intimal tear.The luminal plane of the tunica media is entered and dissect which later lead to a creation of false lumen. Aortic dissection is classified according to the Stanford Classification. Stanford classification type A involved ascending aorta while Stanford classification type B involved other part than ascending aorta.
Patient presented with central stabbing, sharp , tearing pain which later radiates to the back /interscapular retrosternum. The pain is continuous and constant. If the disscetion involve the coronary ostia then myocardial infarction may occur. Hemiplegia, dysphasia and paraplegia are associated with dissection that involved the spinal arteries. Mesenteric arteries are associated with abdominal pain.
Patient may also presented with breathlessness, shock , cyanosed and sweating. There will be an unequal pulse and blood pressure on both arms and legs with radio - radial delay or radio- femoral delay. Other complication may include cardiac failure, cardiac tamponade and aortic regurgitation.
The investigation requires may include ECG that reveal ST elevation , Chest X ray that reveals widening of the mediastinum with fluid in the costophrenic angle, MRI, CT scan that may reveal false lumen and echocardiography which is the best investigation method which may shows pericardial effusion.
The treatment of dissection of the thoracic aorta may include the administration of the pain reliever such as diamorphine. This is follow by establishing an intravenous access through the central and arterial line. Fluid replacement therapy is followed by the administration of colloid solution and blood. Cross match 10 unit of blood is required. The next step involved to control the blood pressure which involved the infusion of the sodium nitroprusside or labetalol infusion if no evidence of cardiac failure to maintain the blood pressure 120/80mmHg. Surgical approach is only require in cases where the dissection is type A and medical management, percutaneous treatment or surgical approach is suitable for type B aortic dissection based on the Stanford classification.