Adenomyosis Pain
Adenomyosis Pain
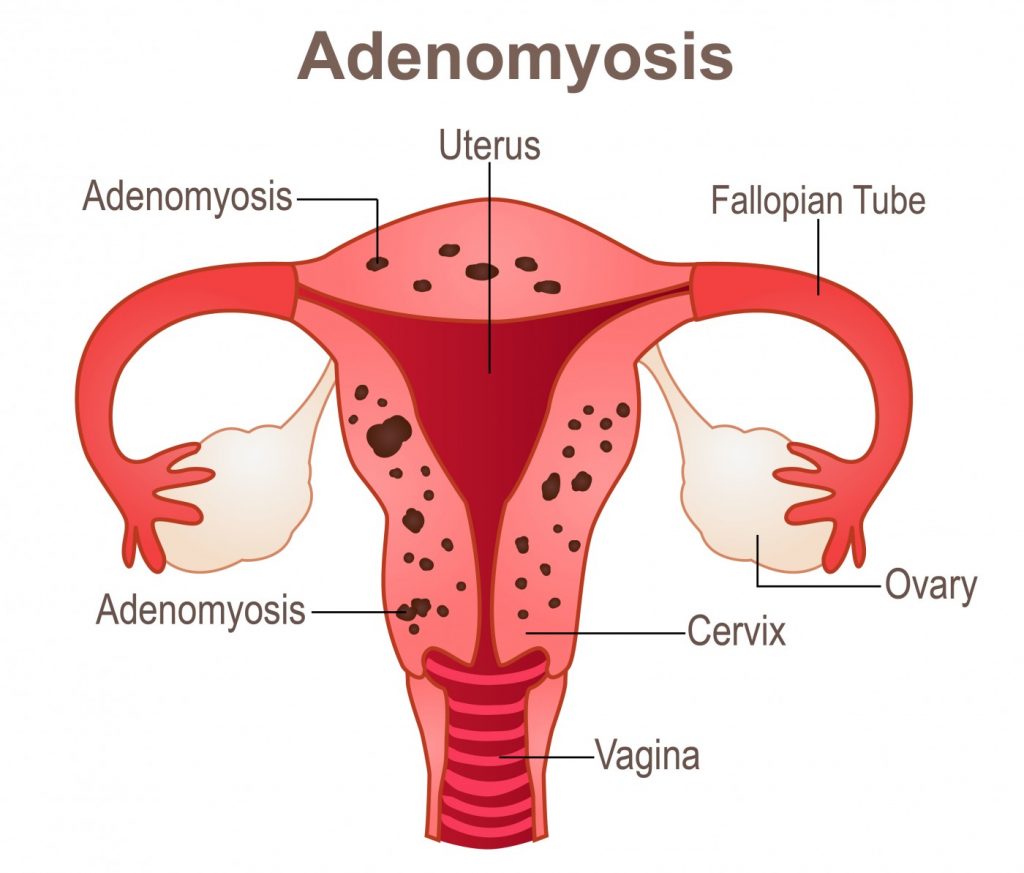
Adenomyosis is an invasion of the endometrium into the myometrium which is benign in nature. Adenomyosis produced a diffusely enlarged uterus. Microscopically, adenomyosis is presented with ectopic non neoplastic endometrial glands and stroma surrounded by hyperplastic and hypertrophic myometrium. In specific case, it may present as circumscribed myometrial mass known as adenomyoma.
Adenomyosis most commonly affects the posterior wall of the uterus. However, the term adenomyosis may also refer to benign hyperplastic change in ampulla of Vater, gallbladder and bile duct.
Adenomyosis usually affect female in the fourth and fifth decade. There are variations among different ethnic groups, race and geographical locations.
It is difficult to get the actual / accurate determination of the true incident due to the variability of the diagnostic criteria. Based on the diagnostic criteria that being used. The incidence of adenomyosis is between 5% and 50%. Women presenting with infertility and pelvic pain have a higher incidence.
Due to variability of the criteria used for diagnosis, an accurate determination of prevalence is difficult. The prevalence is reported to be from 50% - 70%.
What is adenomyosis? It is an abnormal invagination or ingrowth of the basal endometrium into the junctional zone.
Adenomyosis may lead to bleeding, pain and infertility. This is due to the aberration of the sex steroid hormones, altered proliferation of the cells, inflammation and nueroangiogenesis.
In case of adenomyosis, the junctional zone may consists of a region of morphologic dysfunction and structural weakness with susceptibility to invagination of endometrial stromal cells. The junctional zone environment is modulated by increase pressure in the uterine due to leiomyomas or pregnancy. This made it more susceptible to invagination of the endometrial stromal cells.
Other theories of the pathogenesis of adenomyosis include metaplasia theory, Mullerian remnants theory, tissue remodeling theory, multipotental perivascular theory, epithelial -mesenchymal transitional theory, hyperproliferation of uterine smooth muscle cell theory and mast cell activation theory.
In metaplasia theory, adenomyosis is associated with metaplasia of myometrial smooth muscle cells. Mullerian remnants theory, adenomyosis is linked with de novo development from Muullerian rests in myometrium.
In tissue remodeling theory, the ectopic endometrial tissue of the adenomyosis arises from tissue remodeling due to physiology trauma to the uterus such as spontaneous abortion, childbirth or menstruation or due to iatrogenic trauma to the uterine such as during uterine surgery.
In multipotential perivascular stem cells theory, adenomyosis is due to the pathophysiologic vascular remodeling and angiogenesis. This lead to vascular smooth muscle hypertrophy, proliferation and later migration.
Increased in estrogen concentration may lead to enhanced growth of the endometriuam and angiogenesis and invagination into the junctional zone. This is known as epithelial – mesochymal transition theory.
In women with adneomyosis, the hyperproliferative uterine smooth muscle cells has been connected with activation of the MAPK/ EPK pathway. This is called as hyperproliferation of uterine smooth muscle cell theory.
The severity of the adenomyosis is indicated with the present of nerve growth factor which is a mast cell derived mediators. The mast cell mediators lead to differentiation and development of myometrium and maintenance of the adenomyosis. This is known as mast cell activation theory.
Based on the DNA microarray and proteomics analysis, it is revealed that the specific genes which are expressly differentiation in adenomyosis matched the eutopic endometrium. It is suggested that epigenetic and genetic abnormalities lead to the pathogenesis of the adenomyosis.
The risk factors of developing adenomyosis are age which is more than 35 years old, treatment by tamoxifen, multiparity and other less common causes such as smoking and previous uterine surgery.
Adenomyosis is associated with urinary tract dysfunction, endometrial polyps, endometriosis, uterine fibroids, and leiomyomas.
MRI and biopsies of the uterus and endometrium are useful in diagnosing adenomyosis. Patient may present with enlarged uterus, dysmenorrhea and pelvic pain.
Patient with adenomyosis may appear asymptomatic or present with non specific symptoms. The most common symptoms are chronic pelvic pain, dysmenorrhea, menorrhagia and abnormal uterine bleeding. Patient may develop urinary tract symptoms such as urge urinary incontinence, daytime frequency and stress urinary incontinence. On physical examination, the uterus may appear tender and enlarged.
The differential diagnosis of adenomyosis are malignant uterine tumours, benign uterine tumours pregnancy and metastatic diseases.
The investigation needed for detection of adenomyosis include imaging technique and biopsy.
There are 2 forms of imaging techniques such as transvaginal ultrasound and MRI. The initial test for evaluation of suspected adenomyosis is the transvaginal ultrasound with sensitivity of 72%-82.5% and specificity of 81%=84%. Transvaginal ultrasound can be two or three dimensional. Three-dimensional transvaginal ultrasound able to provide the junctional zone thickness. Transvaginal ultrasound with power colour flow Doppler can differentiate between leiomyoma and adenomyosis.
MRI is considered as a more sensitive imaging technique than transvaginal ultrasound with sensitivity of 77%-93% and specificity of 67%-99%.However it is not the ideal first line of diagnostic tool due to its higher cost of the procedure.
The other tests include uterine biopsy with histological interpretation and hysterectomy with histologic interpretation as well as uterine sparing operative treatment with histologic interpretation.
The characteristic of adenomyosis based on 2-dimensional transvaginal sonographic marker may include the enlargement of the uterus, thickening of the uterine wall, cystic anechoic space or lakes in the myometrium, heterogeneous echo texture, thickening of the transition zone and obscure endometrial /myometrial border as well as thickening of the transitional zone. In 3 dimensional TVUS a junctional zone maximum is more than 8 mm and minimum is more than 4mm.
On MRI, adenomyosis may present with low density widening of the junctional zone on T2 –weighted images, which relates to the thickening of junctional zone and hyperplasia of the smooth muscle.
3 objectives parameter for MRI diagnosis of adneomyosis are thickening of the junctional zone to at least 8-12mm, junctional max/ total myometrium is more than 40% and junctional zone max – junctional zone min is more than 5mm.
The most practicable way to establish the diagnosis of adenomyosis is the histological interpretation of uterine biopsy. The pathological interpretation of uterine biopsy may reveal the present of endometrial glands and stromal elements within the myometrium. However, there is problem with biopsy artifact and sampling bias.
Pathological interpretation of the uterine sparing operative treatment or hysterectomy with histological evaluation also pose its own problems.
The diagnostic difficulty in marcellated specimens arises due to the modification of the spatial arrangement of the tissue which leads to difficulty in referencing the surface. Another issue is the sampling bias . The criteria also vary among the pathologists regarding the depth of invasions.
The mainstay treatment for adenomyosis is surgical therapy. Hysterectomy is curative, The uterine sparing operative treatment is an option for those who wish not to undergo hysterectomy and preserve fertility. There are two forms of uterine sparing operative treatments. These are uterine sparing operative treatment excisional techniques and non excisional technique. Uterine sparing operative treatment excisional techniques involve complete excision ( adenmyomectomy) or cytoreduction ( partial adenomyomectomy).
Uterine sparing treatment non excisional technique include laparoscopic techniques such as uterine artery ligation and electrocoagulation , hysteroscopic techniques such as endometrial ablation or endomyometrial resection, MRI or ultrasound guided high frequency ultrasound ablation ( high intensity focused ultrasound), uterine artery embolization ( UAE), microwave ablation, radiofrequency ablation for focal adenomyosis, thermoablation, and non alcoholic instillation ( cystic adenomyosis).
High intensity frequency ultrasound, and uterine artery emboliation is offer as the most encouraging results
Medication may include continuous use of oral contraceptive pills, selective progesterone receptor modulator and high dose progestins which temporarily improve the symptoms.
Adenomyosis regression may temporarily induce by danazol, Gnrha, aromatase inhibitor and levonogestrol releasing intrauterine device.
Adenomyosis symptoms usually resolves after the menopause. It is a benign proliferative of endometrial tissue. The complications of adenomyosis are increased risk of malignant disease and anemia from loss of blood associated with heavy periods.