|
|
Pathology definition - Ulcerative Colitis
Ulcerative colitis
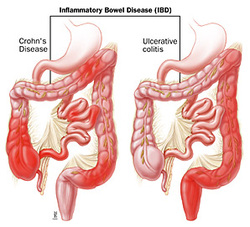
Ulcerative colitis is part of the inflammatory bowel disease which also include Crohn’s disease.
Ulcerative colitis is presented with dysplastic changes of the epithelium. There are ulcers and crypt abscess due to infiltration of the neutrophil in the crypt lumen. In later case, there will be an atrophy of the gland and fibrosis of the submucosal. There will also be a mononuclear inflammatory infiltration of the lamina propria.
Ulcerative colitis may present with remnants of mucosal from previous case of ulceration. This is presented as friable pseudopolyps of the mucosal. Ulcerative colitis involved the rectum and characterized as continuous lesions of the colon. There will be a loss of haustrations which lead to lead pipe appearance of the colon.
Ulcerative colitis mostly affect women and occur due to impairment in the regulation of the immune system.
Patient who suffer from ulcerative colitis may complain of chronic case of bloody diarrhea and mucous. Patient may also complain of tenesmus. Tenesmus is an urge to defecate without any sufficient straining.Patient may also present with toxic megacolon which is inflammation of the myenteric plexuses that lead to gangrenous colon. There might also be an incidence of intestinal obstruction as a result of severe stenosis with increase risk of developing colorectal adenocarcinoma. Ulcerative colitis may cause portal hypertension from the effect of fibrosing chronic cholestasis which is known as primary sclerosing cholangitis. Dermatological condition such as pyoderma gangrenosum may also be associated with ulcerative colitis.
The treatment of ulcerative colitis may include steroids such as glucocorticoids, anti inflammatory drugs such as sulfasalazine or surgical procedure such as proctocolectomy with placement of ileostomy as well as antibiotic /nutritional support and anti diarrheal medication.
References
1.Lennard-Jones, J. E. “Classification of Inflammatory Bowel Disease.” Research-article, July 8, 2009.
2.Warren S, and Sommers SC. “PAthology of Regional Ileitis and Ulcerative Colitis.” Journal of the American Medical Association 154, no. 3 (January 16, 1954): 189–193. doi:10.1001/jama.1954.02940370001001.
Ulcerative colitis is part of the inflammatory bowel disease which also include Crohn’s disease.
Ulcerative colitis is presented with dysplastic changes of the epithelium. There are ulcers and crypt abscess due to infiltration of the neutrophil in the crypt lumen. In later case, there will be an atrophy of the gland and fibrosis of the submucosal. There will also be a mononuclear inflammatory infiltration of the lamina propria.
Ulcerative colitis may present with remnants of mucosal from previous case of ulceration. This is presented as friable pseudopolyps of the mucosal. Ulcerative colitis involved the rectum and characterized as continuous lesions of the colon. There will be a loss of haustrations which lead to lead pipe appearance of the colon.
Ulcerative colitis mostly affect women and occur due to impairment in the regulation of the immune system.
Patient who suffer from ulcerative colitis may complain of chronic case of bloody diarrhea and mucous. Patient may also complain of tenesmus. Tenesmus is an urge to defecate without any sufficient straining.Patient may also present with toxic megacolon which is inflammation of the myenteric plexuses that lead to gangrenous colon. There might also be an incidence of intestinal obstruction as a result of severe stenosis with increase risk of developing colorectal adenocarcinoma. Ulcerative colitis may cause portal hypertension from the effect of fibrosing chronic cholestasis which is known as primary sclerosing cholangitis. Dermatological condition such as pyoderma gangrenosum may also be associated with ulcerative colitis.
The treatment of ulcerative colitis may include steroids such as glucocorticoids, anti inflammatory drugs such as sulfasalazine or surgical procedure such as proctocolectomy with placement of ileostomy as well as antibiotic /nutritional support and anti diarrheal medication.
References
1.Lennard-Jones, J. E. “Classification of Inflammatory Bowel Disease.” Research-article, July 8, 2009.
2.Warren S, and Sommers SC. “PAthology of Regional Ileitis and Ulcerative Colitis.” Journal of the American Medical Association 154, no. 3 (January 16, 1954): 189–193. doi:10.1001/jama.1954.02940370001001.
