Emergency Strategy - How to treat urinary tract fistula
Emergency Strategy - How to treat urinary fistula
Patient is admitted to the hospital if he suffered from acute emergencies due to malignancy or gastrointestinal disease ( causes of urinary fistula), the patient unable to take oral antibiotics and suffer from sepsis.
After the patient has been stabilized with proper evaluation of the airway, breathing and circulation, consider IV antibiotics , pressor or IV fluid bolus to treat urosepsis.
In case of ureterovaginal fistula , urethrovaginal fistula and vesicovaginal fistula, foley catheter is placed. If urinary tract infection is suspected consider IV broad spectrum antibiotics. For further treatment , opinion from gynecologist or urologist is required.
In case of colovesical fistula, culture is obtained. In case of urinary tract infection, broad spectrum antibiotic is commence once the infection is approved. Surgical treatment may be required in certain cases.
Patient will finally discharge if there is no evidence of sepsis and able to ingest oral antibiotics with follow up at the urinary and gynecology clinic.
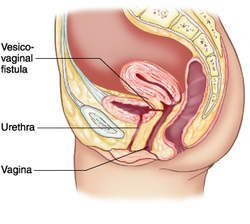
Vesicovaginal fistula may present as leakage of the urine from the vagina constantly. Vesicovaginal fistula may present due to radiation therapy or after removal of foley catheter post surgical procedure. Continuous flow of urinary drainage may also occur with vesicovaginal fistula.
Colovesical fistula may affect the patient and cause diarrhea, abdominal pain ( suprapubic region), recurrent or chronic urinary tract infection and hematuria, fecaluria, pnueumaturia, malodorous urine and debris/food particles in the urine.
Ureterovaginal fistula may present as urinary drainage through vagina constantly and present post operatively other signs include flank abdominal pain and low grade fever due to renal obstruction and urinoma.
Vaginal urinary drainage or asymptomatic are common presentation of urethrovaginal fistula. Symptoms usually depends on the location and sizes of the fistula. Positional and intermittent urinary discharge is associated with ureterovesical fistula.
On physical examination, speculum may reveal small reddened area of granulomatous tissue on the opening of the fistula. This commonly present due to ureterovaginal fistula, urethrovaginal fistula and vesicovaginal fistula.
Obtain past medical history, surgical history and obstetric history. Patient is evaluated for any signs and symptoms of urinary tract infection, Crohn’s disease, malignancy and renal obstruction.
The differential diagnosis may include recurrent urinary tracy infection, diabetic urine fermentation, urinary tract instrumentation, clostridia involvement in case of colovesical fistula . Vaginitis, normal discharge from the vagina and urinary incontinence are the differential diagnosis for ureterovaginal fistula, urethrovaginal fistula and vesicovaginal fistula.
The investigations require are urinalysis ( present of white blood cell, debris and bacteria in colovesical fistula and white blood cell and bacteria in urethrovaginal, ureterovaginal and vesicovaginal fistula), creatinine and blood urea nitrogen ( abnormal if renal obstruction).
Imaging technique is useful and include CT scan of the pelvis and abdomen with contrast in colovesical fistula. Voiding cystourethrography or cystoscopy is useful for vesicovaginal fistula.
Voiding cystourethrography is useful for urethrovaginal fistula while cystoscopy and intravenous pyelogram for ureterovaginal fistula.
Double dye test is performed to confirm the present of ureterovaginal fistula, urethrovaginal fistula and vesicovaginal fistula. Tampon is used. Then the patient will take oral phenazopyridine. Methylene blue will be instilled to the bladder. Distal blue discoloration of the tampon after 1 hour suggestive of urethrovaginal fistula. Vesicovaginal fistula is suggested by midportion blue discoloration while yellow orange tampon is suggesitve of ureterovaginal fistula.
Black particle after administration of activated charcoal may occur due to colovesical fistula.
What is urinary fistula? It is a connection that is form between the urinary tract and organ in the pelvis, abdomen cavity , skin and thoracic cavity.
Urinary tract fistula is divided into colovesical fistula, urethrovaginal fistula, ureterovaginal fistula and vesicovaginal fistula.
Colovesical fistula common in men and mostly occur due to exposure to radiation, Crohn’s disease, carcinoma of the colon and bladder, trauma to the pelvis, diverticular disease and consequences of gastrointestinal disease.
Vesicovaginal fistula , ureterovaginal fistula and urethrovaginal fistula commonly present due to iatrogenic causes such as injury to the structures during pelvic surgery, urologic surgery or gynecology surgery. Besides that trauma due to obstetric causes and difficulty /obstructed labor may also lead to urinary fistula.
References
1.We, Goodwin, and Scardino Pt. “Vesicovaginal and Ureterovaginal Fistulas: a Summary of 25 Years of Experience.” The Journal of Urology 123, no. 3 (March 1980): 370–374.
2.Pontari, M A, M A McMillen, R H Garvey, and G H Ballantyne. “Diagnosis and Treatment of Enterovesical Fistulae.” The American Surgeon 58, no. 4 (April 1992): 258–263.
3.Michelassi, F, M Stella, T Balestracci, F Giuliante, P Marogna, and G E Block. “Incidence, Diagnosis, and Treatment of Enteric and Colorectal Fistulae in Patients with Crohn’s Disease.” Annals of Surgery 218, no. 5 (November 1993): 660–666.
Patient is admitted to the hospital if he suffered from acute emergencies due to malignancy or gastrointestinal disease ( causes of urinary fistula), the patient unable to take oral antibiotics and suffer from sepsis.
After the patient has been stabilized with proper evaluation of the airway, breathing and circulation, consider IV antibiotics , pressor or IV fluid bolus to treat urosepsis.
In case of ureterovaginal fistula , urethrovaginal fistula and vesicovaginal fistula, foley catheter is placed. If urinary tract infection is suspected consider IV broad spectrum antibiotics. For further treatment , opinion from gynecologist or urologist is required.
In case of colovesical fistula, culture is obtained. In case of urinary tract infection, broad spectrum antibiotic is commence once the infection is approved. Surgical treatment may be required in certain cases.
Patient will finally discharge if there is no evidence of sepsis and able to ingest oral antibiotics with follow up at the urinary and gynecology clinic.
Vesicovaginal fistula may present as leakage of the urine from the vagina constantly. Vesicovaginal fistula may present due to radiation therapy or after removal of foley catheter post surgical procedure. Continuous flow of urinary drainage may also occur with vesicovaginal fistula.
Colovesical fistula may affect the patient and cause diarrhea, abdominal pain ( suprapubic region), recurrent or chronic urinary tract infection and hematuria, fecaluria, pnueumaturia, malodorous urine and debris/food particles in the urine.
Ureterovaginal fistula may present as urinary drainage through vagina constantly and present post operatively other signs include flank abdominal pain and low grade fever due to renal obstruction and urinoma.
Vaginal urinary drainage or asymptomatic are common presentation of urethrovaginal fistula. Symptoms usually depends on the location and sizes of the fistula. Positional and intermittent urinary discharge is associated with ureterovesical fistula.
On physical examination, speculum may reveal small reddened area of granulomatous tissue on the opening of the fistula. This commonly present due to ureterovaginal fistula, urethrovaginal fistula and vesicovaginal fistula.
Obtain past medical history, surgical history and obstetric history. Patient is evaluated for any signs and symptoms of urinary tract infection, Crohn’s disease, malignancy and renal obstruction.
The differential diagnosis may include recurrent urinary tracy infection, diabetic urine fermentation, urinary tract instrumentation, clostridia involvement in case of colovesical fistula . Vaginitis, normal discharge from the vagina and urinary incontinence are the differential diagnosis for ureterovaginal fistula, urethrovaginal fistula and vesicovaginal fistula.
The investigations require are urinalysis ( present of white blood cell, debris and bacteria in colovesical fistula and white blood cell and bacteria in urethrovaginal, ureterovaginal and vesicovaginal fistula), creatinine and blood urea nitrogen ( abnormal if renal obstruction).
Imaging technique is useful and include CT scan of the pelvis and abdomen with contrast in colovesical fistula. Voiding cystourethrography or cystoscopy is useful for vesicovaginal fistula.
Voiding cystourethrography is useful for urethrovaginal fistula while cystoscopy and intravenous pyelogram for ureterovaginal fistula.
Double dye test is performed to confirm the present of ureterovaginal fistula, urethrovaginal fistula and vesicovaginal fistula. Tampon is used. Then the patient will take oral phenazopyridine. Methylene blue will be instilled to the bladder. Distal blue discoloration of the tampon after 1 hour suggestive of urethrovaginal fistula. Vesicovaginal fistula is suggested by midportion blue discoloration while yellow orange tampon is suggesitve of ureterovaginal fistula.
Black particle after administration of activated charcoal may occur due to colovesical fistula.
What is urinary fistula? It is a connection that is form between the urinary tract and organ in the pelvis, abdomen cavity , skin and thoracic cavity.
Urinary tract fistula is divided into colovesical fistula, urethrovaginal fistula, ureterovaginal fistula and vesicovaginal fistula.
Colovesical fistula common in men and mostly occur due to exposure to radiation, Crohn’s disease, carcinoma of the colon and bladder, trauma to the pelvis, diverticular disease and consequences of gastrointestinal disease.
Vesicovaginal fistula , ureterovaginal fistula and urethrovaginal fistula commonly present due to iatrogenic causes such as injury to the structures during pelvic surgery, urologic surgery or gynecology surgery. Besides that trauma due to obstetric causes and difficulty /obstructed labor may also lead to urinary fistula.
References
1.We, Goodwin, and Scardino Pt. “Vesicovaginal and Ureterovaginal Fistulas: a Summary of 25 Years of Experience.” The Journal of Urology 123, no. 3 (March 1980): 370–374.
2.Pontari, M A, M A McMillen, R H Garvey, and G H Ballantyne. “Diagnosis and Treatment of Enterovesical Fistulae.” The American Surgeon 58, no. 4 (April 1992): 258–263.
3.Michelassi, F, M Stella, T Balestracci, F Giuliante, P Marogna, and G E Block. “Incidence, Diagnosis, and Treatment of Enteric and Colorectal Fistulae in Patients with Crohn’s Disease.” Annals of Surgery 218, no. 5 (November 1993): 660–666.

