Emergency Strategy - How to treat cardiac tamponade
Emergency Strategy - How to treat cardiac tamponade
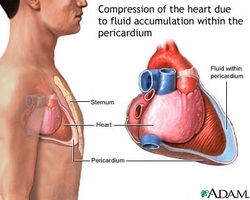
What is cardiac tamponade? Cardiac tamponade is a cardiac compression which is hemodynamically significant and caused by pericardial effusion.
The causes of cardiac tamponade are autoimmune disease ( rheumatic fever, drug reactions, serum sickness, collagen disease- SLE, rheumatoid arthritis, idiopathic relapsing pericarditis and post infarction, post, pericardiotomy), metabolic ( hypothyroidism, uremia), infection( fungal, pyogenic bacteria, TB, viral influenza and coxsackie), hemopericardium ( post cardiac pacing, catheterization, trauma, surgery, aortic dissection and cardiac rupture), neoplastic( lymphoma, lung carcinoma), radiotherapy and myocardial infarction.
Cardiac tamponade is associated with Beck’s triad ( small quiet heart sound, low blood pressure and raised jugular venous pressure). The characteristic of pleural effusion such as impalpable apex beat, dullness over the area of the pericardium, muffled heart sounds and the present of third heart sound are also associated with cardiac tamponade . There will be an increase in the pressure in the pulmonary vein and systemic veins. This will characterized as raised jugular venous pressure , rapid ‘y’ descent, crepitation , wheezing, orthopnea, tachypnea and Kussmaul’s sign ( high jugular venous pressure with inspiration). Pulsus paradoxus ( fall of systolic arterial pressure of more than 10 mmHg on inspiration than expiration confirms the present of pulsus paradoxus), poorly perfused peripheries, small pulse pressure, hypotension and tachycardia are indications of decrease in cardiac output which is related to cardiac tamponade . Patient also may complain of chest pain in precordial region and dyspnea.
The investigations require are ECG, chest x ray and echocardiography . ECG may present with electrical alternans / alternating morphology of QRS complex or low voltage complex sinus tachycardia. Chest x ray may be normal in cases of acute tamponade or presented with large globular heart, Echocardiography may reveal large effusion , wide variation in inflow velocities of tricuspid or mitral valves during the respiration and diastolic collapse of the right atrium and right ventricles.
Management include treatment of the underlying disorders. Volume expansion is considered. The preload is increased by increasing venous pressure with administration of isotonic fluid before parenteral inotropic support. Inotropic agent are also considered before the next treatment is considered.
Echocardiography is performed before pericardiocentesis. The success of pericardiocentesis is determined by the sizes of the effusion. Pericardiocentesis will not be complicated and successful if the sizes of the pericardial effusion is 10 mm or more. Pericardiocentesis is performed in case of purulent effusion, TB or malignancy is suspected or when the circulation is affected in case of effusion which collected rapidly. In traumatic cases , urgent thoracotomy is done . Surgery is not delay.
In non traumatic but severe cases, wide bore needle is inserted directly inwards and medial slightly in the fourth to fifth intercostal space which is 1cm to 2cm medial to the cardiac dullness left border . Make sure fluid is obtained.
In non traumatic cases, consider subxiphoid technique. Echocardiography, is useful with apical and lateral approach based on the sites of effusion. In subxiphoid technique, the needle ( 14- 18 gauge) is inserted while the patient is 45 degree sit up to the left xiphocostal angle and at angle 30 degree, the needle is advanced towards the left sides of the shoulder. Aspiration is performed and continue until fluid is gained. In certain cases, the effusion may be hemorrhagic. It is important to differentiate between hemorrhagic effusion and intracardiac blood. The blood from intracardium will be clot after a few mililiters are placed in the glass tube. However hemorrhagic effusion will not.
Aspiration needle can be attached to the V lead terminal on the cable of the ECG in an attempt to reduce the chances of entering the cardiac chamber. After aspiration to dryness, free drainage is facilitate using the pericardial drain in situ. Aspiration fluid is sent for culture, cytology, gram stain and biochemical studies. The pericardial drain will be removed after 24 hour when the fluid drainage has been stopped. It is important to avoid contraindicated drug such as nitrates, diuretics or preload reducing agents.
References
1.Spodick, David H. “Acute Cardiac Tamponade.” New England Journal of Medicine 349, no. 7 (2003): 684–690. doi:10.1056/NEJMra022643.
2.Guberman, B. A., N. O. Fowler, P. J. Engel, M. Gueron, and J. M. Allen. “Cardiac Tamponade in Medical Patients.” Circulation 64, no. 3 (September 1, 1981): 633–640. doi:10.1161/01.CIR.64.3.633.
3.Alcan KE, Zabetakis PM, Marino ND, Franzone AJ, Michelis MF, and Bruno MS. “MAnagement of Acute Cardiac Tamponade by Subxiphoid Pericardiotomy.” JAMA 247, no. 8 (February 26, 1982): 1143–1148. doi:10.1001/jama.1982.03320330039023.
What is cardiac tamponade? Cardiac tamponade is a cardiac compression which is hemodynamically significant and caused by pericardial effusion.
The causes of cardiac tamponade are autoimmune disease ( rheumatic fever, drug reactions, serum sickness, collagen disease- SLE, rheumatoid arthritis, idiopathic relapsing pericarditis and post infarction, post, pericardiotomy), metabolic ( hypothyroidism, uremia), infection( fungal, pyogenic bacteria, TB, viral influenza and coxsackie), hemopericardium ( post cardiac pacing, catheterization, trauma, surgery, aortic dissection and cardiac rupture), neoplastic( lymphoma, lung carcinoma), radiotherapy and myocardial infarction.
Cardiac tamponade is associated with Beck’s triad ( small quiet heart sound, low blood pressure and raised jugular venous pressure). The characteristic of pleural effusion such as impalpable apex beat, dullness over the area of the pericardium, muffled heart sounds and the present of third heart sound are also associated with cardiac tamponade . There will be an increase in the pressure in the pulmonary vein and systemic veins. This will characterized as raised jugular venous pressure , rapid ‘y’ descent, crepitation , wheezing, orthopnea, tachypnea and Kussmaul’s sign ( high jugular venous pressure with inspiration). Pulsus paradoxus ( fall of systolic arterial pressure of more than 10 mmHg on inspiration than expiration confirms the present of pulsus paradoxus), poorly perfused peripheries, small pulse pressure, hypotension and tachycardia are indications of decrease in cardiac output which is related to cardiac tamponade . Patient also may complain of chest pain in precordial region and dyspnea.
The investigations require are ECG, chest x ray and echocardiography . ECG may present with electrical alternans / alternating morphology of QRS complex or low voltage complex sinus tachycardia. Chest x ray may be normal in cases of acute tamponade or presented with large globular heart, Echocardiography may reveal large effusion , wide variation in inflow velocities of tricuspid or mitral valves during the respiration and diastolic collapse of the right atrium and right ventricles.
Management include treatment of the underlying disorders. Volume expansion is considered. The preload is increased by increasing venous pressure with administration of isotonic fluid before parenteral inotropic support. Inotropic agent are also considered before the next treatment is considered.
Echocardiography is performed before pericardiocentesis. The success of pericardiocentesis is determined by the sizes of the effusion. Pericardiocentesis will not be complicated and successful if the sizes of the pericardial effusion is 10 mm or more. Pericardiocentesis is performed in case of purulent effusion, TB or malignancy is suspected or when the circulation is affected in case of effusion which collected rapidly. In traumatic cases , urgent thoracotomy is done . Surgery is not delay.
In non traumatic but severe cases, wide bore needle is inserted directly inwards and medial slightly in the fourth to fifth intercostal space which is 1cm to 2cm medial to the cardiac dullness left border . Make sure fluid is obtained.
In non traumatic cases, consider subxiphoid technique. Echocardiography, is useful with apical and lateral approach based on the sites of effusion. In subxiphoid technique, the needle ( 14- 18 gauge) is inserted while the patient is 45 degree sit up to the left xiphocostal angle and at angle 30 degree, the needle is advanced towards the left sides of the shoulder. Aspiration is performed and continue until fluid is gained. In certain cases, the effusion may be hemorrhagic. It is important to differentiate between hemorrhagic effusion and intracardiac blood. The blood from intracardium will be clot after a few mililiters are placed in the glass tube. However hemorrhagic effusion will not.
Aspiration needle can be attached to the V lead terminal on the cable of the ECG in an attempt to reduce the chances of entering the cardiac chamber. After aspiration to dryness, free drainage is facilitate using the pericardial drain in situ. Aspiration fluid is sent for culture, cytology, gram stain and biochemical studies. The pericardial drain will be removed after 24 hour when the fluid drainage has been stopped. It is important to avoid contraindicated drug such as nitrates, diuretics or preload reducing agents.
References
1.Spodick, David H. “Acute Cardiac Tamponade.” New England Journal of Medicine 349, no. 7 (2003): 684–690. doi:10.1056/NEJMra022643.
2.Guberman, B. A., N. O. Fowler, P. J. Engel, M. Gueron, and J. M. Allen. “Cardiac Tamponade in Medical Patients.” Circulation 64, no. 3 (September 1, 1981): 633–640. doi:10.1161/01.CIR.64.3.633.
3.Alcan KE, Zabetakis PM, Marino ND, Franzone AJ, Michelis MF, and Bruno MS. “MAnagement of Acute Cardiac Tamponade by Subxiphoid Pericardiotomy.” JAMA 247, no. 8 (February 26, 1982): 1143–1148. doi:10.1001/jama.1982.03320330039023.

