Hepatic Abscess
Hepatic Abscess
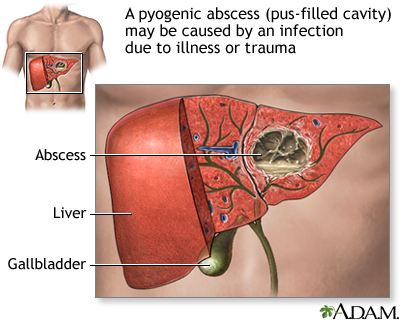
Liver abscess is also known as pyogenic hepatic abscess or amebic hepatic abscess.
Liver abscess is a necrotic infection of the liver usually classified as pyogenic or amebic.
Pyogenic liver abscess is usually polymicrobial (Klebsiella pneumoniae [43%], Escherichia
coli [33%], Streptococcus spp. [37%], Pseudomonas aeruginosa, Proteus spp.,Bacteroides
spp. [24%], Fusobacterium spp., Actinomyces spp., gram-positive anaerobes,and Staphylococcus aureus).
Pyogenic liver abscess occurs from :
-Diverticulitis or appendicitis with spread via the portal circulation.
-Infection by way of portal system (portal pyemia).
-Hematogenous spread via the hepatic artery, though uncommon; if a solitary organism is
isolated, a distant source of hematogenous seeding should be sought.
-Biliary disease with cholangitis (accounts for approximately 40% to 60%).
-Cryptogenic.
-Gallbladder disease with contiguous spread to the liver.
-Penetrating wounds.
-Amebic hepatic abscess is caused by the parasite Entamoeba histolytica. Amebiasis is
usually due to fecal-oral contamination and invades the intestinal mucosa, gaining entry
into the portal system to reach the liver.
The symptoms and signs of liver abscess are fever, chills, and sweats,weakness/malaise,anorexia with weight loss, nausea, vomiting, and diarrhea, cough with pleuritic chest pain, right upper quadrant abdominal pain,hepatomegaly,splenomegaly,jaundice,pleural effusions, rales, and friction rubs may
be present.Most abscesses occur on the right lobe of the liver
The differential diagnosis of liver abscess are diverticulitis, cholecystitis,cholangitis, pancreatitis, appendicitis, perforated viscus, mesenteric ischemia and pulmonary embolism.
Features suggesting an amebic cause include travel to an endemic area, single abscess
rather than multiple abscesses, subacute onset of symptoms, and absence of conditions predisposing to pyogenic liver abscess.
Common laboratory investigations are complete blood count which may reveal leukocytosis, liver function test may include alkaline phosphatase which is
most commonly elevated (95% to 100%); aspartate transaminase (AST) and alanine
transaminase (ALT) elevated in 50% of cases; elevated bilirubin (28% to 30%) and decreased albumin.
Prothrombin time (INR): prolonged (70%), blood cultures: positive in 50% of cases aspiration (50% sterile), Stool samples for E. histolytica trophozoites
(positive in 10% to 15% of amebic liver abscess cases) and serologic testing for E. histolytica does not differentiate acute from old infections.
Ultrasound (80% to 100% sensitivity in detecting abscesses) shows round or oval hypoechogenic mass. CT scan is more sensitive in detecting hepatic abscesses and contiguous organ extension and is the imaging study of choice. Chest x-ray: abnormal in 50% of the cases, may reveal elevated right hemidiaphragm, subdiaphragmatic air-fluid levels, pleural effusions and consolidating infiltrates. Most liver abscesses are single; however, multiple liver abscesses can occur with systemic bacteremia.
The management of pyogenic liver abscess differs from that of amebic liver abscess.Medical management is the cornerstone of therapy in amebic liver abscess, whereas early intervention in the form of surgical therapy or catheter drainage and parenteral
antibiotics is the rule in pyogenic liver abscess.
Percutaneous drainage under CT or ultrasound guidance is essential in the treatment of pyogenic liver abscesses. Aspiration of hepatic amebic abscesses is not required unless there is no response to treatment or a pyogenic cause is being considered. Empiric broad-spectrum antibiotics are recommended initially until culture results are available.
If fever persists for 2 wk despite percutaneous drainage and antibiotic therapy as outlined or if there is failure of aspiration or failure of percutaneous drainage, surgery is indicated.
In patients not responding to intravenous antibiotics and percutaneous drainage, hepatic artery antibiotic infusion can be considered.
In patients with evidence of metastatic disease that is causing biliary obstruction, a gastroenterology consultation for endoscopic retrograde cholangiopancreatography and stenting should be considered.
Follow-up imaging should be used to monitor response to therapy; continue treatment until CT scan shows complete or near complete resolution of cavity.
Liver abscess is also known as pyogenic hepatic abscess or amebic hepatic abscess.
Liver abscess is a necrotic infection of the liver usually classified as pyogenic or amebic.
Pyogenic liver abscess is usually polymicrobial (Klebsiella pneumoniae [43%], Escherichia
coli [33%], Streptococcus spp. [37%], Pseudomonas aeruginosa, Proteus spp.,Bacteroides
spp. [24%], Fusobacterium spp., Actinomyces spp., gram-positive anaerobes,and Staphylococcus aureus).
Pyogenic liver abscess occurs from :
-Diverticulitis or appendicitis with spread via the portal circulation.
-Infection by way of portal system (portal pyemia).
-Hematogenous spread via the hepatic artery, though uncommon; if a solitary organism is
isolated, a distant source of hematogenous seeding should be sought.
-Biliary disease with cholangitis (accounts for approximately 40% to 60%).
-Cryptogenic.
-Gallbladder disease with contiguous spread to the liver.
-Penetrating wounds.
-Amebic hepatic abscess is caused by the parasite Entamoeba histolytica. Amebiasis is
usually due to fecal-oral contamination and invades the intestinal mucosa, gaining entry
into the portal system to reach the liver.
The symptoms and signs of liver abscess are fever, chills, and sweats,weakness/malaise,anorexia with weight loss, nausea, vomiting, and diarrhea, cough with pleuritic chest pain, right upper quadrant abdominal pain,hepatomegaly,splenomegaly,jaundice,pleural effusions, rales, and friction rubs may
be present.Most abscesses occur on the right lobe of the liver
The differential diagnosis of liver abscess are diverticulitis, cholecystitis,cholangitis, pancreatitis, appendicitis, perforated viscus, mesenteric ischemia and pulmonary embolism.
Features suggesting an amebic cause include travel to an endemic area, single abscess
rather than multiple abscesses, subacute onset of symptoms, and absence of conditions predisposing to pyogenic liver abscess.
Common laboratory investigations are complete blood count which may reveal leukocytosis, liver function test may include alkaline phosphatase which is
most commonly elevated (95% to 100%); aspartate transaminase (AST) and alanine
transaminase (ALT) elevated in 50% of cases; elevated bilirubin (28% to 30%) and decreased albumin.
Prothrombin time (INR): prolonged (70%), blood cultures: positive in 50% of cases aspiration (50% sterile), Stool samples for E. histolytica trophozoites
(positive in 10% to 15% of amebic liver abscess cases) and serologic testing for E. histolytica does not differentiate acute from old infections.
Ultrasound (80% to 100% sensitivity in detecting abscesses) shows round or oval hypoechogenic mass. CT scan is more sensitive in detecting hepatic abscesses and contiguous organ extension and is the imaging study of choice. Chest x-ray: abnormal in 50% of the cases, may reveal elevated right hemidiaphragm, subdiaphragmatic air-fluid levels, pleural effusions and consolidating infiltrates. Most liver abscesses are single; however, multiple liver abscesses can occur with systemic bacteremia.
The management of pyogenic liver abscess differs from that of amebic liver abscess.Medical management is the cornerstone of therapy in amebic liver abscess, whereas early intervention in the form of surgical therapy or catheter drainage and parenteral
antibiotics is the rule in pyogenic liver abscess.
Percutaneous drainage under CT or ultrasound guidance is essential in the treatment of pyogenic liver abscesses. Aspiration of hepatic amebic abscesses is not required unless there is no response to treatment or a pyogenic cause is being considered. Empiric broad-spectrum antibiotics are recommended initially until culture results are available.
If fever persists for 2 wk despite percutaneous drainage and antibiotic therapy as outlined or if there is failure of aspiration or failure of percutaneous drainage, surgery is indicated.
In patients not responding to intravenous antibiotics and percutaneous drainage, hepatic artery antibiotic infusion can be considered.
In patients with evidence of metastatic disease that is causing biliary obstruction, a gastroenterology consultation for endoscopic retrograde cholangiopancreatography and stenting should be considered.
Follow-up imaging should be used to monitor response to therapy; continue treatment until CT scan shows complete or near complete resolution of cavity.