Emergency Strategy - How to treat retinal artery occlusion
Emergency Strategy - How to treat occlusion of the retinal artery
After initial step of patient ‘s airway, breathing, circulation, disability and exposure assessment, treatment should begin immediately. The aim of the immediate treatment is to preserve and restore the sights of the affected eye. The aim of therapy will focus on improving blood flow by dilation of the artery, removing the embolus in the blood vessel by dislodging the emboli and improving the gradient of perfusion by reducing the intra ocular pressure . Bear in mind that irreversible loss of vision may occur if no treatment is given within 90 minutes time interval.
The globe of the eye is massaged. Patient is asked to close the eyelid and lie supine. Pressure is applied to the eye for every 15 seconds for 5 cycles with resting interval lasting also for 15 seconds. The aim of this digital massage of the globe of the eye is to dislodge the emboli. Establish the IV lines and considered IV heparin to prevent formation of clot/thrombus. Aspirin is used as an alternatives. Thrombus or clot may be lysed by intra - arterial fibrinolysis. Intra ocular pressure need to be reduced. Consider, topical application of timolol or IV acetazolamide or paracentesis of anterior chamber. If patient develop inflammatory arteritis consider high dose of systemic steroid. The retinal vessel may be dilated by increasing partial pressure of carbon dioxide by asking the patient to breath in and out of the paper bag.
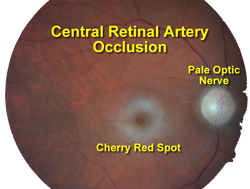
Patient with retinal artery occlusion may present with painless, sudden monocular loss of vision. Physical examination may reveal decrease in visual acuity significantly and afferent pupillary defect. Fundoscopic examination of the retinal may reveal cherry red spot over the fovea, “ Hollenhorst plaque” or glinting yellow or white flecks within the vessel and visualization of the emboli within the vascular tree of the retinal vessel. Besides that edematous ischemic lesion will also be visible. Opacification of the transparent retinal nerve layer may also occur due to occlusion. Visual field testing may reveal loss of visual field in one eye but partial loss of visual field is associated with occlusion involving just branches of the retinal artery. Other test include measurement of the intraocular pressure.
The common differential diagnosis of retinal artery occlusion are optic neuritis, acute angle closure glaucoma, central retinal vein occlusion and temporal arteritis.
The investigations required are full blood count, urea and electrolytes, partial thromboplastin time, prothrombin time, glucose, C reactive protein, ESR, blood urea nitrogen, creatinine, rheumatoid factor, ANA, serum protein and hemoglobin electrophoresis. The imaging technique require are fluorescein angiography, carotid artery doppler studies, carotid artery ultrasound, electroretinography and echocardiography in selected cardio related cases.
Occlusion of the retinal artery is associated with history of atherosclerotic disease, diabetes mellitus, hypertension, coronary artery disease, valvular heart disease, vasculitis ( lupus) or sickle cell disease. Central retinal artery occlusion is the most common caused. The obstruction/occlusion of retinal artery is cause by thrombotic, embolic, inflammatory, reduction in perfusion and spasm of the artery.
The thrombotic causes include Sickle cell disease/hypercoagulable state or from the rupture of the pre- existing atherosclerotic plaque intravascularly.
Embolic causes of occlusion of the retinal artery are due to dissection of the carotid artery and ophthalmic artery, atrial myxoma, stenosis of the carotid artery, atherosclerotic plaque and cardiogenic emboli from the valvular heart disease.
Vasculitis, lupus erythematous and temporal arteritis are associated with inflammatory causes of occlusion of the retinal artery. Drug such as cocaine or migraine headache is associated with spasm of the artery which may lead to occlusion of the retinal artery. Retrobulbar hemorrhage, acute angle closure glaucoma and hypotension are common condition based on high pressure and low flow which later lead to decrease in perfusion.
References
1.Mangat, Harpal S. “Retinal Artery Occlusion.” Survey of Ophthalmology 40, no. 2 (September 1995): 145–156.
2.Schumacher, M., D. Schmidt, and A. K. Wakhloo. “Intra-arterial Fibrinolytic Therapy in Central Retinal Artery Occlusion.” Neuroradiology 35, no. 8 (October 1, 1993): 600–605. doi:10.1007/BF00588405.
3.Nh, Atebara, Brown Gc, and Cater J. “Efficacy of Anterior Chamber Paracentesis and Carbogen in Treating Acute Nonarteritic Central Retinal Artery Occlusion.” Ophthalmology 102, no. 12 (December 1995): 2029–34; discussion 2034–5.
4.Rumelt, Shimon, Yosef Dorenboim, and Uri Rehany. “Aggressive Systematic Treatment for Central Retinal Artery Occlusion.” American Journal of Ophthalmology 128, no. 6 (December 1999): 733–738.
After initial step of patient ‘s airway, breathing, circulation, disability and exposure assessment, treatment should begin immediately. The aim of the immediate treatment is to preserve and restore the sights of the affected eye. The aim of therapy will focus on improving blood flow by dilation of the artery, removing the embolus in the blood vessel by dislodging the emboli and improving the gradient of perfusion by reducing the intra ocular pressure . Bear in mind that irreversible loss of vision may occur if no treatment is given within 90 minutes time interval.
The globe of the eye is massaged. Patient is asked to close the eyelid and lie supine. Pressure is applied to the eye for every 15 seconds for 5 cycles with resting interval lasting also for 15 seconds. The aim of this digital massage of the globe of the eye is to dislodge the emboli. Establish the IV lines and considered IV heparin to prevent formation of clot/thrombus. Aspirin is used as an alternatives. Thrombus or clot may be lysed by intra - arterial fibrinolysis. Intra ocular pressure need to be reduced. Consider, topical application of timolol or IV acetazolamide or paracentesis of anterior chamber. If patient develop inflammatory arteritis consider high dose of systemic steroid. The retinal vessel may be dilated by increasing partial pressure of carbon dioxide by asking the patient to breath in and out of the paper bag.
Patient with retinal artery occlusion may present with painless, sudden monocular loss of vision. Physical examination may reveal decrease in visual acuity significantly and afferent pupillary defect. Fundoscopic examination of the retinal may reveal cherry red spot over the fovea, “ Hollenhorst plaque” or glinting yellow or white flecks within the vessel and visualization of the emboli within the vascular tree of the retinal vessel. Besides that edematous ischemic lesion will also be visible. Opacification of the transparent retinal nerve layer may also occur due to occlusion. Visual field testing may reveal loss of visual field in one eye but partial loss of visual field is associated with occlusion involving just branches of the retinal artery. Other test include measurement of the intraocular pressure.
The common differential diagnosis of retinal artery occlusion are optic neuritis, acute angle closure glaucoma, central retinal vein occlusion and temporal arteritis.
The investigations required are full blood count, urea and electrolytes, partial thromboplastin time, prothrombin time, glucose, C reactive protein, ESR, blood urea nitrogen, creatinine, rheumatoid factor, ANA, serum protein and hemoglobin electrophoresis. The imaging technique require are fluorescein angiography, carotid artery doppler studies, carotid artery ultrasound, electroretinography and echocardiography in selected cardio related cases.
Occlusion of the retinal artery is associated with history of atherosclerotic disease, diabetes mellitus, hypertension, coronary artery disease, valvular heart disease, vasculitis ( lupus) or sickle cell disease. Central retinal artery occlusion is the most common caused. The obstruction/occlusion of retinal artery is cause by thrombotic, embolic, inflammatory, reduction in perfusion and spasm of the artery.
The thrombotic causes include Sickle cell disease/hypercoagulable state or from the rupture of the pre- existing atherosclerotic plaque intravascularly.
Embolic causes of occlusion of the retinal artery are due to dissection of the carotid artery and ophthalmic artery, atrial myxoma, stenosis of the carotid artery, atherosclerotic plaque and cardiogenic emboli from the valvular heart disease.
Vasculitis, lupus erythematous and temporal arteritis are associated with inflammatory causes of occlusion of the retinal artery. Drug such as cocaine or migraine headache is associated with spasm of the artery which may lead to occlusion of the retinal artery. Retrobulbar hemorrhage, acute angle closure glaucoma and hypotension are common condition based on high pressure and low flow which later lead to decrease in perfusion.
References
1.Mangat, Harpal S. “Retinal Artery Occlusion.” Survey of Ophthalmology 40, no. 2 (September 1995): 145–156.
2.Schumacher, M., D. Schmidt, and A. K. Wakhloo. “Intra-arterial Fibrinolytic Therapy in Central Retinal Artery Occlusion.” Neuroradiology 35, no. 8 (October 1, 1993): 600–605. doi:10.1007/BF00588405.
3.Nh, Atebara, Brown Gc, and Cater J. “Efficacy of Anterior Chamber Paracentesis and Carbogen in Treating Acute Nonarteritic Central Retinal Artery Occlusion.” Ophthalmology 102, no. 12 (December 1995): 2029–34; discussion 2034–5.
4.Rumelt, Shimon, Yosef Dorenboim, and Uri Rehany. “Aggressive Systematic Treatment for Central Retinal Artery Occlusion.” American Journal of Ophthalmology 128, no. 6 (December 1999): 733–738.

