Emergency Strategy - How to treat hypoglycemia
Emergency Strategy - How to treat hypoglycemia
What is hypoglycemia? There is no clear/ absolute definition of hypoglycemia. The characteristic of the symptoms are based on the absolute level of glucose and the rate of fall of the level of glucose to that level. Treatment is usually begins when the blood glucose level is less than 3.9 mmol/l ( the threshold for treatment is varies ).
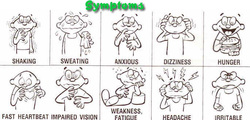
The symptoms and signs of hypoglycemia are pin and needles in the tongue and lips, hunger, palpitation, sweating, trembling and shaking. Patient will fulfill the characteristic of Whipple triad such as symptoms associate with hypoglycemia, low plasma glucose level ( < 3.9 mmol/l) and raised plasma glucose will improve the symptoms. Patient may also present with neuroglycopenia which consists of transient ischemic attacks, stroke ( focal neurological deficit), coma, behavioral changes, difficulty in concentrating, seizures and confusion as well as stupor.
Patient should be admitted to hospital if there are high risk of recurrent hypoglycemia or prolonged hypoglycemia. Other reasons for admission include previous history of hypoglycemia , unable to be discharge to care giver, unable to self care, patient with significant renal or liver impairment, elderly ( > than 60 years old ), frail patient with poor social support and poor oral intake, patient with recurrent episodes of hypoglycemia for the last 2 weeks and patient with glibenclamide ( IV dextrose is needed).
The common causes of hypoglycemia are sepsis, liver failure, cardiac failure frail, elderly and renal failure. Other causes are intake of oral hypoglycemic agent or insulin . Oral hypoglycemia agent and insulin may lead to hypoglycemic in cases of accidental overdose or intentional purpose. Renal failure will lead to hypoglycemic if due to decrease clearance of the oral hypoglycemic agents and insulin. Other factors which contributes to hypoglycemia are intensive insulin therapy , wrong or excess doses or ill timing of administration of insulin or oral hypoglycemic agent. Drugs such as glucagon, alcohols, salicylate, pentamidine , gatifloxacin, and quinine may also lead to hypoglycemia. Patient currently on insulin may develop relative therapeutic excess of insulin due to increase sensitivity to insulin as a result of weight loss or increase physical activity. or missed meals which lead to hypoglycemia.
Non islet cell tumors or insulinoma as well as hormonal disturbance such as myxedema , Addison’s disease, deficiency of growth hormone may also lead to hypoglycemia.
Generally correction of plasma glucose should be done as quickly as possible. Patient is given simple and complex carbohydrate ( 15 -2 mg ). These includes, 3 teaspoons of glucose, 1-2 tablets of sweets and glucose, orange juice, pieces of fruit, 1-2 pieces of sandwich /bread and 3 pieces of crackers. After 15 minutes the procedure is repeated if blood glucose less than 4 mmol/l . Subsequent food intake is important to prevent relapse.
If the patient is unconscious with impairment of mental function consider it as an emergency case. IV lines are set. Patient is turn to the left lateral position. 25- 50 ml 50% dextrose IV followed by saline flush is given. This procedure is repeated every 10 - 15 minutes until blood glucose is normal and mental function is recovered. This is follow later by glucose drink or 5 - 10% of DW infusion if the patient is fully conscious. 10% of dextrose drips are continued if hypoglycemia us due to overdose of oral hypoglycemic agent or long acting insulin.
Difficulty in establishing IV access may lead to administration of 1 mg glucagon IM or deep subcutaneous ( SC).After the patient regain consciousness.
What is hypoglycemia? There is no clear/ absolute definition of hypoglycemia. The characteristic of the symptoms are based on the absolute level of glucose and the rate of fall of the level of glucose to that level. Treatment is usually begins when the blood glucose level is less than 3.9 mmol/l ( the threshold for treatment is varies ).
The symptoms and signs of hypoglycemia are pin and needles in the tongue and lips, hunger, palpitation, sweating, trembling and shaking. Patient will fulfill the characteristic of Whipple triad such as symptoms associate with hypoglycemia, low plasma glucose level ( < 3.9 mmol/l) and raised plasma glucose will improve the symptoms. Patient may also present with neuroglycopenia which consists of transient ischemic attacks, stroke ( focal neurological deficit), coma, behavioral changes, difficulty in concentrating, seizures and confusion as well as stupor.
Patient should be admitted to hospital if there are high risk of recurrent hypoglycemia or prolonged hypoglycemia. Other reasons for admission include previous history of hypoglycemia , unable to be discharge to care giver, unable to self care, patient with significant renal or liver impairment, elderly ( > than 60 years old ), frail patient with poor social support and poor oral intake, patient with recurrent episodes of hypoglycemia for the last 2 weeks and patient with glibenclamide ( IV dextrose is needed).
The common causes of hypoglycemia are sepsis, liver failure, cardiac failure frail, elderly and renal failure. Other causes are intake of oral hypoglycemic agent or insulin . Oral hypoglycemia agent and insulin may lead to hypoglycemic in cases of accidental overdose or intentional purpose. Renal failure will lead to hypoglycemic if due to decrease clearance of the oral hypoglycemic agents and insulin. Other factors which contributes to hypoglycemia are intensive insulin therapy , wrong or excess doses or ill timing of administration of insulin or oral hypoglycemic agent. Drugs such as glucagon, alcohols, salicylate, pentamidine , gatifloxacin, and quinine may also lead to hypoglycemia. Patient currently on insulin may develop relative therapeutic excess of insulin due to increase sensitivity to insulin as a result of weight loss or increase physical activity. or missed meals which lead to hypoglycemia.
Non islet cell tumors or insulinoma as well as hormonal disturbance such as myxedema , Addison’s disease, deficiency of growth hormone may also lead to hypoglycemia.
Generally correction of plasma glucose should be done as quickly as possible. Patient is given simple and complex carbohydrate ( 15 -2 mg ). These includes, 3 teaspoons of glucose, 1-2 tablets of sweets and glucose, orange juice, pieces of fruit, 1-2 pieces of sandwich /bread and 3 pieces of crackers. After 15 minutes the procedure is repeated if blood glucose less than 4 mmol/l . Subsequent food intake is important to prevent relapse.
If the patient is unconscious with impairment of mental function consider it as an emergency case. IV lines are set. Patient is turn to the left lateral position. 25- 50 ml 50% dextrose IV followed by saline flush is given. This procedure is repeated every 10 - 15 minutes until blood glucose is normal and mental function is recovered. This is follow later by glucose drink or 5 - 10% of DW infusion if the patient is fully conscious. 10% of dextrose drips are continued if hypoglycemia us due to overdose of oral hypoglycemic agent or long acting insulin.
Difficulty in establishing IV access may lead to administration of 1 mg glucagon IM or deep subcutaneous ( SC).After the patient regain consciousness.

