|
|
Pathology definition - Cerebral Infarction
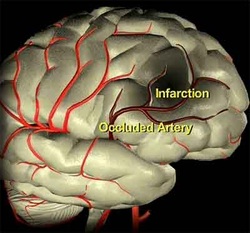
Cerebral infarction
Cerebral infarction is also known as ischemic stroke. There are a few forms of cerebral infarction. These are lacunar infarction, hemorrhagic infarction, non hemorrhagic infarction and border zone infarction. Cerebral infarction /ischemic stroke is treated with thrombolytic therapy within 3 hours of onset.
Lacunar infarction may present with gliosis surrounding small cavitation. Lacunar infarction is due to the obstruction of many small vessels. Hemorrhagic infarction occurs due to the reabsorption of the blood that seeps into infarction. Hemorrhagic infarction is caused by embolism.
Non hemorrhagic infarction will occur through a few stages. Non hemorrhagic infarction is caused by thrombosis. During the first 12 hours, there will be eosinophilic cytoplasm and nuclear pyknosis due to the changes as a result of ischemic neuron. Two days later, infiltration of the microglia and monocytes will be prominent. This will lead to reactive astrocytes and fluid filled cavity or liquefactive necrosis by 3 weeks later. Several months later will be followed by formation of scar tissue known as gliosis.
Border zone infarction is known as wedge shaped infarction and commonly affecting the are between anterior cerebral artery and middle cerebral artery. Border zone infarction is associated with hypotension.
The most common causes of cerebral infarction are embolism, thrombosis and atherosclerosis. Hemorrhage and septic shock may also cause cerebral infarction due to hypotension.
Patient with cerebral infarction may present with multiple symptoms and signs based on the sites of occlusion. Occlusion of the posterior communicating artery may lead to macular sparing homonymous hemianopia and contralateral loss of sensation.
Occlusion of the anterior communicating artery may lead to loss of sensation and weakness of the contralateral leg. Contralateral striate arteries occlusion may lead to contralateral paralysis. Aphasia, homonymous hemianopia and contralateral loss of sensation and paralysis will lead to occlusion of the middle cerebral artery.
References
1.Pickering, George. “Pathogenesis of Myocardial and Cerebral Infarction: Nodular Arteriosclerosis.” British Medical Journal 1, no. 5382 (February 29, 1964): 517–529.
2.Adams HP, Jr, Butler MJ, Biller J, and Toffol GJ. “NOnhemorrhagic Cerebral Infarction in Young Adults.” Archives of Neurology 43, no. 8 (August 1, 1986): 793–796. doi:10.1001/archneur.1986.00520080041017.
3.Hornig, C. R., W. Dorndorf, and A. L. Agnoli. “Hemorrhagic Cerebral Infarction--a Prospective Study.” Stroke 17, no. 2 (March 1, 1986): 179–185. doi:10.1161/01.STR.17.2.179.
Cerebral infarction is also known as ischemic stroke. There are a few forms of cerebral infarction. These are lacunar infarction, hemorrhagic infarction, non hemorrhagic infarction and border zone infarction. Cerebral infarction /ischemic stroke is treated with thrombolytic therapy within 3 hours of onset.
Lacunar infarction may present with gliosis surrounding small cavitation. Lacunar infarction is due to the obstruction of many small vessels. Hemorrhagic infarction occurs due to the reabsorption of the blood that seeps into infarction. Hemorrhagic infarction is caused by embolism.
Non hemorrhagic infarction will occur through a few stages. Non hemorrhagic infarction is caused by thrombosis. During the first 12 hours, there will be eosinophilic cytoplasm and nuclear pyknosis due to the changes as a result of ischemic neuron. Two days later, infiltration of the microglia and monocytes will be prominent. This will lead to reactive astrocytes and fluid filled cavity or liquefactive necrosis by 3 weeks later. Several months later will be followed by formation of scar tissue known as gliosis.
Border zone infarction is known as wedge shaped infarction and commonly affecting the are between anterior cerebral artery and middle cerebral artery. Border zone infarction is associated with hypotension.
The most common causes of cerebral infarction are embolism, thrombosis and atherosclerosis. Hemorrhage and septic shock may also cause cerebral infarction due to hypotension.
Patient with cerebral infarction may present with multiple symptoms and signs based on the sites of occlusion. Occlusion of the posterior communicating artery may lead to macular sparing homonymous hemianopia and contralateral loss of sensation.
Occlusion of the anterior communicating artery may lead to loss of sensation and weakness of the contralateral leg. Contralateral striate arteries occlusion may lead to contralateral paralysis. Aphasia, homonymous hemianopia and contralateral loss of sensation and paralysis will lead to occlusion of the middle cerebral artery.
References
1.Pickering, George. “Pathogenesis of Myocardial and Cerebral Infarction: Nodular Arteriosclerosis.” British Medical Journal 1, no. 5382 (February 29, 1964): 517–529.
2.Adams HP, Jr, Butler MJ, Biller J, and Toffol GJ. “NOnhemorrhagic Cerebral Infarction in Young Adults.” Archives of Neurology 43, no. 8 (August 1, 1986): 793–796. doi:10.1001/archneur.1986.00520080041017.
3.Hornig, C. R., W. Dorndorf, and A. L. Agnoli. “Hemorrhagic Cerebral Infarction--a Prospective Study.” Stroke 17, no. 2 (March 1, 1986): 179–185. doi:10.1161/01.STR.17.2.179.
