|
|
|
Emergency Strategy - How to treat acute bronchitis
Emergency Strategy - How to treat acute bronchitis
The treatment of acute bronchitis may involve adult related approach and pediatric related approach. Acute bronchitis is treated initially with stabilization of the airway, breathing and circulation. Oxygen need to be supplied adequately mostly if the patient is hypoxic. Look for any evidence of airway obstruction and try to relief the obstruction ( endotracheal intubation). Assess for any signs of dehydration and consider the administration of fluid. Bronchodilator /beta adrenergic agonist is considered in case the patient develop airway obstruction ( proof by wheezing).
Acute bronchitis is usually related to viral infection while chronic bronchitis is mostly due to cigarette smoking and form part of chronic obstructive pulmonary disease. The treatment may include zanamivir or oseltamivir. Symptomatic treatment with cough suppressant, analgesic and antipyretic are also considered.In case of history of influenza A consider amantadine. Antibiotic is not considered due to its side effect and development of resistance. It is only considered if there is an evidence recurrence.
Acute bronchitis in pediatric setting may require a few adjustments. Acetaminophen is considered instead of aspirin for analgesic. Antibiotic should be considered. Any hypoxic child should be treated with oxygen and fluid is considered in case of dehydration. Acute bronchitis may have significant impact in term of morbidity in immunocompromised patient. Therefore careful assessment and evaluation is required.
Patient will be discharged if the symptoms and signs are gone and no respiratory compromise or respiratory complication develop. Patient will require plenty of bed rest, increase in fluid intake and analgesic such as acetaminophen ( children) and aspirin in adults. In high risk population such as chronic lung disease sufferer, old people and immunocompromised consider yearly influenza vaccinations. If shortness of breath develop in 2- 3 weeks time consider referral to hospital ( recurrence of infection).
Patient with acute bronchitis may present with symptoms and signs such as coryza, sore throat, chills myalgias and malaise. These symptoms and signs may precede the upper respiratory tract infection. Patient then, will develop the symptoms of upper respiratory tract infection such as dry non productive cough which later progress into mucopurulent cough. The cough is accompany by chest pain ( burning in characteristic ) and patient will develop shortness of breath ( dyspnea). Coughing blood ( hemoptysis) , wheezing, tachypnea, fever/pyrexia are common signs. Chest examination may reveal rales or rhonci.
The common differential diagnosis of bronchitis may include ( in chronic case) , bronchogenic carcinoma, gastro esophageal reflux disease, bronchiectasis, carcinomatosis, asthma, aspiration, left ventricular failure and sarcoidosis. Acute cases of bronchitis is commonly mistaken for acute sinusitis, occupational exposure, pneumonia, bacterial tracheitis and reactive airway disease.
The investigations require are full blood count ( leukocytosis), bacterial culture, viral culture, PCR testing and chest x ray as well as pulmonary function test.
Bronchitis main etiologies are influenza A and B, rhinovirus, echovirus, parainfluenza, respiratory syncytial virus, adenovirus, coxsackie virus , herpes virus, measles and human meta pneumovirus. Other etiologies are due to infection such as from Bordetella pertussis ( consider erythromycin antibiotic), chlamydia pneumonia and mycoplasma pneumonia.
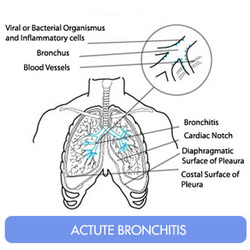
Bronchitis may lead to airway obstruction from the spasm of the bronchial muscle, secretion of the mucopurulent exudates and edematous and erythematous mucous membrane. Bronchitis is also associated with disruption of the cilia, phagocytes and lymphatic functions.
References
1.Verheij, T. J. M., A. A. Kaptein, and J. D. Mulder. “Acute Bronchitis: Aetiology, Symptoms and Treatment.” Family Practice 6, no. 1 (March 1, 1989): 66–69. doi:10.1093/fampra/6.1.66.
2.Nyquist A, Gonzales R, Steiner JF, and Sande MA. “ANtibiotic Prescribing for Children with Colds, Upper Respiratory Tract Infections, and Bronchitis.” JAMA 279, no. 11 (March 18, 1998): 875–877. doi:10.1001/jama.279.11.875.
3.Smucny, J J, L A Becker, R H Glazier, and W McIsaac. “Are Antibiotics Effective Treatment for Acute Bronchitis? A Meta-analysis.” The Journal of Family Practice 47, no. 6 (December 1998): 453–460.
The treatment of acute bronchitis may involve adult related approach and pediatric related approach. Acute bronchitis is treated initially with stabilization of the airway, breathing and circulation. Oxygen need to be supplied adequately mostly if the patient is hypoxic. Look for any evidence of airway obstruction and try to relief the obstruction ( endotracheal intubation). Assess for any signs of dehydration and consider the administration of fluid. Bronchodilator /beta adrenergic agonist is considered in case the patient develop airway obstruction ( proof by wheezing).
Acute bronchitis is usually related to viral infection while chronic bronchitis is mostly due to cigarette smoking and form part of chronic obstructive pulmonary disease. The treatment may include zanamivir or oseltamivir. Symptomatic treatment with cough suppressant, analgesic and antipyretic are also considered.In case of history of influenza A consider amantadine. Antibiotic is not considered due to its side effect and development of resistance. It is only considered if there is an evidence recurrence.
Acute bronchitis in pediatric setting may require a few adjustments. Acetaminophen is considered instead of aspirin for analgesic. Antibiotic should be considered. Any hypoxic child should be treated with oxygen and fluid is considered in case of dehydration. Acute bronchitis may have significant impact in term of morbidity in immunocompromised patient. Therefore careful assessment and evaluation is required.
Patient will be discharged if the symptoms and signs are gone and no respiratory compromise or respiratory complication develop. Patient will require plenty of bed rest, increase in fluid intake and analgesic such as acetaminophen ( children) and aspirin in adults. In high risk population such as chronic lung disease sufferer, old people and immunocompromised consider yearly influenza vaccinations. If shortness of breath develop in 2- 3 weeks time consider referral to hospital ( recurrence of infection).
Patient with acute bronchitis may present with symptoms and signs such as coryza, sore throat, chills myalgias and malaise. These symptoms and signs may precede the upper respiratory tract infection. Patient then, will develop the symptoms of upper respiratory tract infection such as dry non productive cough which later progress into mucopurulent cough. The cough is accompany by chest pain ( burning in characteristic ) and patient will develop shortness of breath ( dyspnea). Coughing blood ( hemoptysis) , wheezing, tachypnea, fever/pyrexia are common signs. Chest examination may reveal rales or rhonci.
The common differential diagnosis of bronchitis may include ( in chronic case) , bronchogenic carcinoma, gastro esophageal reflux disease, bronchiectasis, carcinomatosis, asthma, aspiration, left ventricular failure and sarcoidosis. Acute cases of bronchitis is commonly mistaken for acute sinusitis, occupational exposure, pneumonia, bacterial tracheitis and reactive airway disease.
The investigations require are full blood count ( leukocytosis), bacterial culture, viral culture, PCR testing and chest x ray as well as pulmonary function test.
Bronchitis main etiologies are influenza A and B, rhinovirus, echovirus, parainfluenza, respiratory syncytial virus, adenovirus, coxsackie virus , herpes virus, measles and human meta pneumovirus. Other etiologies are due to infection such as from Bordetella pertussis ( consider erythromycin antibiotic), chlamydia pneumonia and mycoplasma pneumonia.
Bronchitis may lead to airway obstruction from the spasm of the bronchial muscle, secretion of the mucopurulent exudates and edematous and erythematous mucous membrane. Bronchitis is also associated with disruption of the cilia, phagocytes and lymphatic functions.
References
1.Verheij, T. J. M., A. A. Kaptein, and J. D. Mulder. “Acute Bronchitis: Aetiology, Symptoms and Treatment.” Family Practice 6, no. 1 (March 1, 1989): 66–69. doi:10.1093/fampra/6.1.66.
2.Nyquist A, Gonzales R, Steiner JF, and Sande MA. “ANtibiotic Prescribing for Children with Colds, Upper Respiratory Tract Infections, and Bronchitis.” JAMA 279, no. 11 (March 18, 1998): 875–877. doi:10.1001/jama.279.11.875.
3.Smucny, J J, L A Becker, R H Glazier, and W McIsaac. “Are Antibiotics Effective Treatment for Acute Bronchitis? A Meta-analysis.” The Journal of Family Practice 47, no. 6 (December 1998): 453–460.
